Japanese scientists have made a breakthrough in human dental biology by identifying previously unknown dormant third-generation tooth buds that can naturally regrow teeth—challenging the long-standing belief that humans only develop two sets of teeth.
Revolutionizing Dental Science
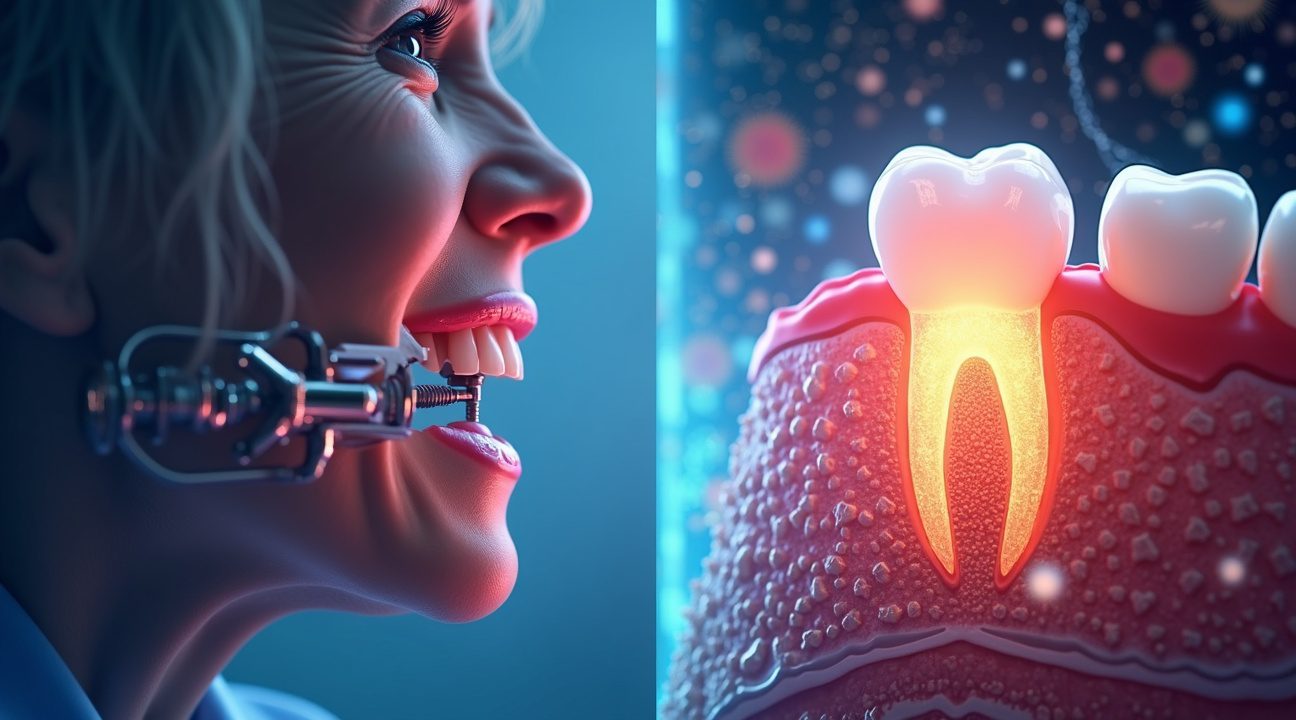
Dr. Katsu Takahashi and his team at the Medical Research Institute Kitano Hospital in Osaka have discovered tooth buds hidden within the human jaw that lie dormant, yet retain the biological potential for natural tooth regeneration. Leveraging these findings, the team developed a novel antibody-based therapy targeting a protein known as USAG-1.
How the Treatment Works
The innovative treatment involves the use of antibodies to suppress the USAG-1 protein—a natural inhibitor of tooth formation. By blocking this protein, the treatment removes the biological restrictions that prevent the hidden third-generation tooth buds from developing into functional teeth.
Key Takeaways
- Discovery of dormant tooth buds: Researchers have identified third-generation tooth buds in the human jaw, refuting the belief that humans develop only two sets of teeth.
- USAG-1 antibody therapy: The treatment reactivates these dormant buds by blocking the suppressive function of the USAG-1 protein.
- Human clinical trials underway: As of October 2024, the groundbreaking therapy entered human testing at Kyoto University Hospital with an initial group of 30 adult male participants.
- Benefits over conventional methods: This regenerative solution provides naturally integrated teeth with sensory feedback and full biological functionality—eliminating the need for costly and high-maintenance alternatives like implants or dentures.
- Broader regenerative potential: The findings pave the way for future developments in organ regeneration and tissue restoration, potentially impacting multiple areas of medicine.
What Lies Ahead
If human trials continue to show success, commercial availability of this revolutionary dental therapy could be expected by 2030. Scientists and clinicians alike are optimistic about the possibilities this discovery opens not just for dentistry, but for broader applications within regenerative medicine.
Hidden Dormant Tooth Buds: The Biological Foundation for Human Tooth Regrowth
The recent discovery by Japanese researchers has fundamentally altered our understanding of human dental biology. Dr. Katsu Takahashi and his team at the Medical Research Institute Kitano Hospital in Osaka have identified something remarkable hiding beneath our gums: dormant third-generation tooth buds that possess the potential for natural tooth regeneration.
Challenging Conventional Dental Wisdom
For decades, dental science operated under the assumption that humans develop only two sets of teeth throughout their lifetime. Primary baby teeth emerge during childhood, followed by permanent adult teeth that replace them. This biological pattern seemed fixed and unchangeable. However, Dr. Takahashi’s research team has uncovered evidence of latent tooth structures that have remained hidden and inactive beneath the gum line.
These third-generation tooth buds represent a complete paradigm shift in how scientists view human dental development. Unlike other mammals that can regenerate teeth multiple times throughout their lives, humans were thought to lack this remarkable ability. The discovery of these dormant structures suggests that the biological machinery for tooth regeneration actually exists within our mouths, waiting for the right conditions to activate.
The Science Behind Latent Teeth
The identification of these dormant tooth buds opens new possibilities for understanding human tooth regeneration mechanisms. These latent teeth contain the same fundamental cellular components found in developing teeth, including dental stem cells and the necessary growth factors. What makes this discovery particularly significant is that these structures have remained viable despite being inactive for potentially decades.
The research team’s findings suggest several important characteristics of these hidden tooth buds:
- They contain multipotent stem cells capable of differentiating into various dental tissues
- The buds maintain their structural integrity even in adult patients
- They possess the genetic programming necessary for complete tooth development
- The dormant state appears to be maintained by specific inhibitory signals
This discovery has profound implications for dental medicine and regenerative therapy. Rather than relying on artificial implants or dentures, future treatments might activate these natural tooth buds to grow replacement teeth. The concept mirrors what scientists have observed in other species, where genetic programming controls complex biological processes.
Dr. Takahashi’s team has also identified the molecular pathways that keep these tooth buds in their dormant state. Understanding these inhibitory mechanisms could lead to targeted therapies that selectively activate tooth regeneration when needed. This represents a significant advancement from current dental treatments, which focus primarily on repair and replacement rather than regeneration.
The presence of third-generation tooth buds challenges our fundamental assumptions about human biology. Just as researchers have made surprising discoveries about brain function and other biological systems, this dental research reveals hidden capabilities within our own bodies.
Current studies focus on determining the optimal conditions for activating these latent teeth while ensuring proper formation and integration with existing dental structures. The research team continues investigating the specific growth factors and signaling molecules required to trigger controlled tooth development from these dormant buds.
This breakthrough represents more than just a scientific curiosity. The discovery of functional third-generation tooth buds provides a concrete biological foundation for developing tooth regeneration therapies. Rather than creating artificial solutions, medical researchers can now work with the body’s existing regenerative capacity to restore lost teeth naturally.
The implications extend beyond individual patient care to broader questions about human evolution and development. These findings suggest that humans retain more regenerative potential than previously recognized, similar to other remarkable biological discoveries that continue reshaping our understanding of life itself.

Revolutionary Drug Mechanism: How USAG-1 Suppression Triggers Natural Tooth Growth
Japanese researchers have developed a groundbreaking approach to tooth regeneration by targeting a specific protein that acts as nature’s brake on dental development. The therapy focuses on USAG-1 (uterine sensitization-associated gene-1), a protein that naturally suppresses the formation of additional teeth beyond our standard two sets. This biological inhibitor prevents the activation of dormant tooth buds that remain hidden within our jaw structures throughout life.
Scientists discovered that by blocking USAG-1’s activity, they could essentially remove the biological handbrakes that prevent tooth regrowth. The human mouth contains dormant third-generation tooth buds that never develop under normal circumstances due to USAG-1’s suppressive effects. These findings represent a significant departure from traditional approaches to tooth replacement, which have relied heavily on artificial implants and prosthetics.
Antibody-Based Treatment Approach
The tooth regeneration drug operates through an antibody-based mechanism that specifically targets and neutralizes USAG-1 proteins. Rather than requiring surgical intervention, this treatment can be administered through simple injection, making it far less invasive than conventional dental procedures. The antibody treatment works by binding to USAG-1 proteins and preventing them from inhibiting natural tooth development pathways.
Key advantages of this antibody approach include:
- Non-surgical administration reduces patient discomfort and recovery time
- Targeted protein suppression minimizes potential side effects on other biological systems
- Injectable format allows for precise dosing and treatment timing
- Reversible mechanism provides safety advantages over permanent genetic modifications
Early animal trials have demonstrated remarkable success with this approach. Mice treated with the USAG-1-blocking antibodies successfully developed new, fully functional teeth that integrated seamlessly with existing dental structures. These regenerated teeth displayed normal root formation, proper enamel development, and complete functionality for chewing and biting.
Ferret studies provided additional validation of the treatment’s effectiveness across different mammalian species. The ferrets’ dental anatomy more closely resembles human tooth structure compared to rodent models, making these results particularly encouraging for potential human applications. Both animal models showed consistent tooth buds activation following treatment, with new teeth emerging within predictable timeframes.
The precision of this antibody treatment distinguishes it from broader genetic therapies that might affect multiple biological pathways simultaneously. By specifically targeting USAG-1, researchers have identified a focused intervention point that appears to trigger natural regenerative processes without disrupting other essential functions. This specificity reduces the likelihood of unintended consequences that often complicate more generalized therapeutic approaches.
Clinical researchers are particularly encouraged by the treatment’s ability to activate dormant biological mechanisms rather than introducing foreign materials or requiring complex surgical procedures. The approach harnesses the body’s existing capacity for tooth development, simply removing the molecular obstacles that prevent this natural process from occurring in adulthood.
The injection-based delivery system offers practical advantages for widespread clinical implementation. Unlike surgical tooth replacement procedures that require specialized facilities and extended recovery periods, this treatment could potentially be administered in standard clinical settings. The non-invasive nature of the therapy also makes it accessible to patients who might not be candidates for traditional implant surgery due to health concerns or anatomical limitations.
Scientists continue to refine the dosing protocols and timing strategies for optimal tooth regeneration outcomes. The ability to control when and how many teeth regenerate through targeted USAG-1 suppression opens possibilities for precise dental restoration that matches individual patient needs. This level of control represents a significant advancement over current regenerative medicine approaches that often produce unpredictable results.
The success of these preclinical models has generated considerable excitement about the potential for human trials. While scientists think they’ve discovered many biological mechanisms in recent years, this particular breakthrough offers immediate practical applications for addressing one of humanity’s most common health challenges.

Human Clinical Trials Launch: 2024 Testing Phase and Path to 2030 Deployment
The groundbreaking tooth regeneration research has officially entered human testing. October 2024 marked a pivotal moment when Kyoto University Hospital launched Phase 1 clinical trials, bringing this revolutionary therapy one step closer to reality.
Current Trial Parameters and Patient Selection
The initial study focuses on a carefully selected group of 30 adult men, ages 30 to 64, who’ve lost at least one tooth. Researchers deliberately chose this demographic to establish baseline safety data before expanding to broader populations. This conservative approach mirrors standard pharmaceutical development protocols, where adult subjects provide initial proof-of-concept data.
Toregem Biopharma, the biotech startup co-founded by Dr. Takahashi, leads both the drug development and eventual commercialization efforts. The company’s strategic partnership with Kyoto University Hospital provides access to world-class research facilities and clinical expertise necessary for these complex trials.
Long-term Vision and Target Population
While current trials focus on adult tooth loss, the therapy’s ultimate goal addresses a much more specific medical need. Researchers plan to treat children born with congenital absence of six or more permanent teeth, a rare genetic condition affecting approximately 0.1% of the population. These children face significant challenges with eating, speaking, and social development throughout their lives.
The pathway from laboratory to clinic represents years of careful scientific progress. Early research identified the mechanisms behind tooth bud formation and the proteins that control this process. Scientists discovered that humans possess dormant tooth buds beyond their typical 32 teeth, similar to how genetic research has revealed hidden biological capabilities in other species.
Current timelines suggest broad availability by 2030, assuming successful completion of all trial phases. This ambitious goal requires clearing multiple regulatory hurdles and demonstrating both safety and efficacy across different patient populations. Phase 1 results will determine whether the therapy moves forward to larger Phase 2 studies, which would test effectiveness in addition to safety.
The commercial implications extend far beyond rare genetic conditions. Successful tooth regeneration could transform dental care for millions who’ve lost teeth due to injury, disease, or aging. Traditional treatments like implants and dentures may eventually give way to biologically grown replacements that integrate naturally with surrounding tissues.
Toregem Biopharma’s approach represents a new frontier in regenerative medicine, where biological processes replace mechanical solutions. The company’s timeline reflects both scientific optimism and realistic assessment of regulatory requirements that govern human therapeutic development.
Natural Teeth vs. Current Dental Solutions: A Revolutionary Alternative
Traditional dental restoration methods have dominated the field for decades, yet each carries significant limitations that impact patients’ quality of life and financial well-being. Dentures frequently slip and cause discomfort, while dental bridges require the alteration of healthy adjacent teeth. Dental implants, though more stable, involve surgical procedures that can cost thousands of dollars per tooth and may fail over time due to infection or bone loss.
The discovery of a third set of hidden teeth capable of regrowth presents a groundbreaking alternative that could fundamentally change how we approach tooth loss. Unlike prosthetic solutions that merely replace missing teeth with artificial materials, this biological approach harnesses the body’s own regenerative capabilities. I find this particularly fascinating because it addresses the root cause of tooth loss rather than simply masking the problem with external devices.
Cost and Invasiveness Comparison
Current dental restoration methods impose substantial financial burdens on patients. A single dental implant can cost between $3,000 to $5,000, while full mouth reconstruction using implants may exceed $40,000. Bridge work, though less expensive initially, often requires replacement every 10–15 years, creating ongoing costs. Dentures present the most affordable option upfront but demand frequent adjustments, relines, and eventual replacement.
The invasiveness of these procedures also creates barriers for many patients:
- Implant surgery requires months of healing time, multiple appointments, and carries risks of nerve damage or sinus complications.
- Bridge preparation involves removing healthy tooth structure from adjacent teeth, permanently weakening them.
- Even well-fitted dentures can cause bone loss over time as they don’t provide the natural stimulation that tooth roots offer to the jawbone.
Natural tooth regrowth through the activation of these hidden dental structures could eliminate many of these concerns. Rather than requiring surgical intervention or tooth modification, this approach would work with the body’s existing biological systems. The potential for genetic breakthroughs in regenerative medicine continues to expand, suggesting that activating dormant tooth buds may become a reality sooner than expected.
Functional and Aesthetic Advantages
Natural teeth provide superior function compared to any artificial alternative. They contain proprioceptive nerves that allow precise bite control and pressure sensitivity, features that no prosthetic can replicate. This sensory feedback helps prevent bite injuries and enables proper chewing mechanics essential for digestion and nutrition.
Aesthetically, naturally regrown teeth would integrate seamlessly with existing dental structures. They’d match the patient’s unique tooth color, shape, and size characteristics without the telltale signs of dental work that often accompany crowns, bridges, or implants. The natural translucency and surface texture of biological teeth cannot be perfectly replicated by artificial materials, regardless of technological advances.
The alignment benefits of natural regrowth also deserve consideration. When teeth grow naturally, they follow the body’s genetic blueprint for proper positioning and spacing. This differs significantly from implants, which must be placed based on available bone structure and may not achieve optimal positioning. Poor implant placement can lead to bite problems, TMJ disorders, and accelerated wear on opposing teeth.
Furthermore, naturally regrown teeth would maintain the dynamic relationship between tooth roots and surrounding bone tissue. This biological connection preserves bone density and gum health in ways that artificial restorations cannot achieve. The discovery reminds me of other remarkable biological phenomena, like how scientists uncover hidden mechanisms within our bodies that we’re only beginning to understand.
The implications extend beyond individual patient benefits. Widespread adoption of natural tooth regrowth could reduce the environmental impact associated with manufacturing dental prosthetics and decrease the medical waste generated by failed implants and worn-out dentures. This biological approach represents a sustainable solution that aligns with the body’s natural healing processes rather than fighting against them.
Critical Challenges: Ensuring Proper Development and Safety
The journey from laboratory success to human application presents significant hurdles that researchers must overcome before tooth regrowth becomes a viable treatment option. While initial studies in animal models have demonstrated promising results, I’ve observed that the transition to human subjects introduces a complex array of considerations that require careful evaluation.
Development and Alignment Complexities
Ensuring that newly formed teeth emerge with proper alignment, appropriate size, and functional structure represents one of the most significant challenges facing regenerative dentistry. The human mouth operates as a precisely calibrated system where each tooth must fit seamlessly with its neighbors while maintaining proper bite mechanics. Current research has shown positive outcomes in mice and ferrets, but these animal models can’t fully replicate the intricate spatial relationships found in human dental anatomy.
Scientists working on this breakthrough technology must address several critical factors during tooth development:
- Precise positioning within the jaw to prevent crowding or spacing issues
- Appropriate size scaling to match existing teeth and maintain bite function
- Proper root formation to ensure adequate anchoring and stability
- Correct orientation to facilitate normal chewing and speaking patterns
- Integration with surrounding tissues including gums and supporting bone structures
The complexity increases when considering that human jaws vary significantly in size and shape between individuals. Unlike standardized laboratory animals, each patient presents unique anatomical challenges that could affect how regenerated teeth develop and integrate.
Safety Protocols and Long-term Monitoring
Translation from animals to humans requires extensive safety evaluations that extend far beyond initial tooth formation. Current clinical trials focus heavily on comprehensive monitoring of side effects and drug efficacy to establish safety profiles before any widespread treatment becomes available. I’ve noted that researchers must track not only immediate reactions but also long-term consequences that might emerge months or years after treatment.
The monitoring process involves multiple phases of evaluation. Early-stage trials examine basic safety parameters and determine optimal dosing protocols. Subsequent phases expand to larger patient groups while tracking tooth function and alignment over extended periods. This methodical approach helps identify potential complications that might not manifest immediately after treatment.
Scientists must also consider how regenerated teeth interact with existing dental work, orthodontic treatments, and ongoing oral health maintenance. The long-term durability of these new teeth remains under evaluation, as researchers need to verify that they can withstand decades of normal use without unexpected complications.
Clinical trial safety protocols require participants to undergo regular examinations using advanced imaging techniques to monitor tooth development progress. These assessments help researchers identify any deviations from normal growth patterns early enough to intervene if necessary. The data collected during these trials will ultimately determine whether this technology can safely transition from experimental treatment to standard dental care.
Current regenerative dentistry challenges extend beyond the immediate treatment phase. Researchers must establish guidelines for patient selection, treatment timing, and post-procedure care that account for individual variations in healing and development. Much like how scientists think they’ve discovered other biological mysteries, understanding tooth regrowth requires patience and systematic investigation.
The success of this revolutionary approach depends on maintaining rigorous safety standards while advancing our understanding of human tooth development. Each clinical trial provides valuable insights that bring researchers closer to offering patients a natural alternative to traditional dental prosthetics. However, the timeline for widespread availability remains dependent on successfully addressing these critical development and safety challenges through continued research and evaluation.

World-First Innovation: Transforming Global Dental Care and Medical Science
Natural tooth regrowth represents a groundbreaking shift from conventional dental treatments, offering patients a biological solution that could eliminate the need for lifelong prosthetic maintenance. I find this development particularly significant because it addresses one of humanity’s most persistent health challenges through regenerative medicine rather than replacement therapy.
Revolutionary Impact on Dental Treatment
This discovery marks the first successful identification of a dormant third set of teeth in humans, fundamentally changing how dental professionals approach tooth loss treatment. Traditional methods require patients to invest thousands of dollars in implants, bridges, or dentures that need regular replacement and adjustment throughout their lives. The ability to regenerate natural teeth could transform this expensive cycle into a one-time biological solution.
Healthcare systems worldwide spend billions annually on dental prosthetics and their ongoing maintenance. Natural regrowth technology could dramatically reduce these costs while providing patients with fully functional teeth that integrate seamlessly with existing oral structures. I believe this innovation will make advanced dental care accessible to populations who currently can’t afford expensive prosthetic options.
Gateway to Advanced Regenerative Medicine
The success of tooth regrowth technology establishes crucial foundations for broader organ regeneration research. Teeth contain multiple tissue types including enamel, dentin, pulp, and supporting structures, making them complex biological systems similar to other organs. Scientists who master tooth regeneration gain valuable insights into stem cell activation, tissue engineering, and controlled biological development.
This breakthrough could accelerate research into regenerating other body parts, from damaged heart tissue to lost limbs. The techniques developed for activating dormant tooth buds may prove applicable to stimulating regenerative processes in various organs. I expect this discovery will attract significant investment and research attention, potentially leading to treatments for conditions that currently have no cure.
The implications extend beyond individual patient care to reshape entire medical fields. Regenerative medicine could:
- Reduce dependency on organ transplants
- Eliminate rejection complications
- Provide treatments using patients’ own biological systems
Just as scientists explore DNA recreation in other contexts, researchers can now investigate how dormant biological programs might be reactivated throughout the human body.
This innovation positions Japan at the forefront of regenerative medicine research, potentially establishing new global standards for biological restoration therapies. The success of natural tooth regrowth could fundamentally alter how medical professionals approach tissue loss and organ failure across multiple specialties.

Sources:
Medical Xpress – Japanese Pioneering Drug to Regrow Teeth
Dimensions of Dental Hygiene – Regrowing Teeth May Be on the Horizon
Dentinova – Can You Really Regrow Teeth? Meet Japan’s New Drug
Dentistry Today – Researchers in Japan Discover Medicine Capable of Regrowing Third Set of Teeth for Humans
Medpath – Japanese Researchers Begin Human Trials for Revolutionary Tooth Regeneration Drug


