Revolution in Fertility Treatment: Robotic IVF Achieves Historic First
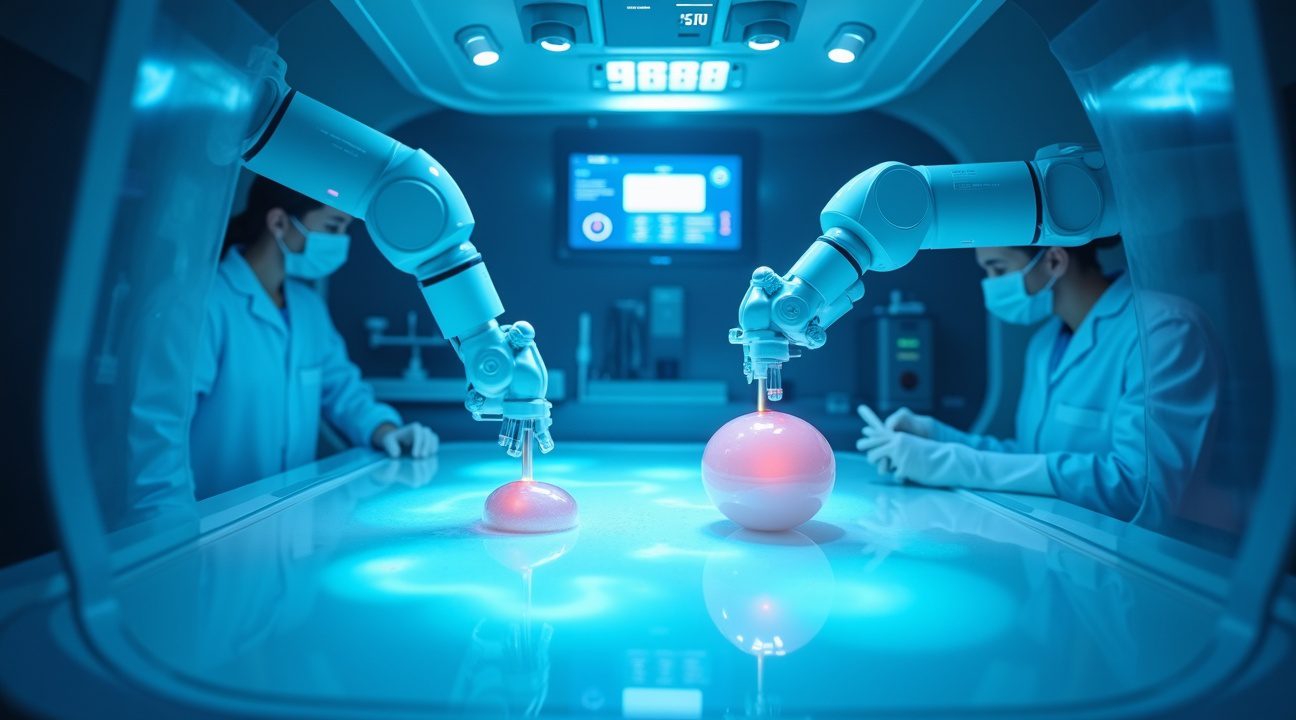
A groundbreaking medical milestone has been achieved with the birth of a baby from an embryo created entirely through robotic IVF technology, marking the first successful case of fully automated embryo creation.
This revolutionary system utilized artificial intelligence and precision robotics to complete 23 intricate steps of the intracytoplasmic sperm injection (ICSI) process, remotely guided by specialists located over 3,700 kilometers away. The achievement demonstrates a significant step forward in reproductive health and medical automation.
Key Takeaways
- Remote Operation Breakthrough: Fertility specialists in New York successfully controlled the entire robotic IVF procedure conducted in a Guadalajara clinic, showcasing how remote technology can transcend geographical barriers in specialized healthcare.
- AI-Powered Automation: The robotic system handled 23 distinct ICSI steps by using artificial intelligence for optimal sperm selection, laser immobilization, and real-time embryo viability assessments with microscopic precision.
- Performance Comparison: Despite a longer procedure time (9 minutes 56 seconds compared to 1 minute 22 seconds for human specialists), robotic systems achieved an impressive 80% fertilization success rate, providing consistent and reliable results devoid of fatigue or human variability.
- Medical Benefits: Automated systems aim to reduce human error, standardize complex procedures, enhance egg survival rates, and potentially lower costs, making fertility treatments more accessible around the world.
- Future Impact: With continued development, this technology could dramatically transform global access to fertility treatments by enabling remote expert oversight while still relying on embryologists for essential decision-making and quality assurance.
To learn more about this pioneering innovation in robotic fertility technology, visit this MIT Technology Review article covering the full story.
How the Robotic ICSI System Works and Its Unprecedented Remote Operation
The revolutionary robotic ICSI system represents a breakthrough in assisted reproductive technology that fundamentally transforms how fertility treatments are performed. Unlike traditional methods where embryologists manually handle every aspect of fertilization, this advanced system relies on artificial intelligence and precision robotics to execute the most delicate procedures with unprecedented accuracy.
This sophisticated technology automates the entire intracytoplasmic sperm injection process through a series of precisely programmed steps. The robotic system begins by selecting the most viable sperm from samples, using AI-powered algorithms to identify optimal candidates based on morphology and motility patterns. Once selected, the robots immobilize the sperm using specialized micro-tools before carefully injecting it directly into the egg’s cytoplasm.
Remote Control Capabilities That Transcend Geographic Boundaries
The most remarkable aspect of this system lies in its remote operation capabilities, which were demonstrated when specialists in New York successfully controlled the entire procedure in a Guadalajara clinic over 3,700 kilometers away. This distance operation showcases how modern technology can overcome geographical limitations in specialized medical care. The remote control system utilizes high-speed internet connections and real-time monitoring to ensure every movement and decision can be precisely executed from thousands of miles away.
I find it fascinating that the system managed to automate 23 distinct steps of the ICSI process, each requiring the kind of precision that typically demands years of specialized training for human embryologists. The robotic arms move with microscopic accuracy, manipulating cells that are barely visible to the naked eye while maintaining the sterile conditions essential for successful fertilization.
The AI component continuously analyzes data throughout the procedure, making split-second decisions about sperm quality, injection timing, and embryo viability. This robotic technology doesn’t just replicate human actions—it enhances them by eliminating hand tremors, reducing human error, and providing consistent performance regardless of fatigue or external pressures.
Despite this extensive automation, certain critical steps remain under human control. Egg and sperm collection procedures still require direct medical intervention, as these processes involve complex interactions with patients that current technology cannot fully replicate. Similarly, embryo transfer continues to be performed manually, ensuring that the final step maintains the human touch essential for successful implantation.
The remote monitoring system provides real-time visual feedback through high-definition cameras and specialized imaging equipment. Operators can observe every microscopic detail of the procedure, adjusting parameters and making decisions as if they were physically present in the laboratory. This capability opens unprecedented possibilities for expert consultation across continents, potentially making advanced fertility treatments accessible in regions with limited specialized expertise.
The success of this remotely operated system demonstrates how AI technology can bridge gaps in medical expertise while maintaining the highest standards of care. The precision of robotic manipulation combined with AI-driven decision-making creates a system that potentially surpasses human capabilities in consistency and accuracy.
This technological advancement also addresses critical challenges in fertility medicine, including the shortage of skilled embryologists and the need for standardized procedures across different clinics. By automating complex tasks while maintaining remote oversight capabilities, the system could revolutionize access to high-quality fertility treatments worldwide.
The implications extend beyond individual treatments to encompass broader healthcare delivery models. Remote operation capabilities suggest a future where specialized medical procedures can be performed anywhere in the world, guided by experts regardless of their physical location. This technological evolution represents a significant step forward in democratizing access to advanced medical care while maintaining the expertise and precision required for successful outcomes.
Advanced AI and Robotic Technologies Behind the Breakthrough
The successful birth represents a convergence of cutting-edge laboratory automation and artificial intelligence that transforms how I approach reproductive medicine. This robotic IVF system integrates sophisticated hardware components with intelligent software algorithms to create an unprecedented level of precision in embryo creation.
Core Hardware Components Driving Automation
The robotic platform incorporates several critical technologies that work in seamless coordination. These include:
- An inverted microscope providing detailed cellular visualization
- A heated stage maintaining optimal temperature conditions for embryo development
- A non-contact laser system for precise sperm immobilization
- A piezo actuator enabling micro-level manipulation accuracy
- A motorized stage allowing automated positioning
- An objective turret facilitating multiple magnification levels
- Oil and air microinjectors for controlled substance delivery
- High-resolution imaging cameras capturing real-time procedural data
AI algorithms serve as the intelligent backbone of this system, making critical decisions that traditionally required human expertise. The software analyzes sperm morphology to identify the most viable candidates for fertilization, eliminating subjective human assessment. Artificial intelligence then controls the laser system to immobilize selected sperm tails with micrometer-level precision, ensuring optimal positioning for injection.
Embryo evaluation represents another breakthrough area where AI excels beyond human capabilities. The system examines chromosome appearance and predicts implantation success rates through advanced pattern recognition algorithms. This automated assessment reduces variability and increases accuracy in determining embryo viability.
The procedural workflow maintains a hybrid approach between automation and human oversight. While robotic systems perform the mechanical actions autonomously, human operators can initiate specific steps remotely. This design ensures safety while maximizing the benefits of automated precision.
Key innovations include AI-powered intracytoplasmic sperm injection (ICSI), which automates the delicate process of inserting sperm directly into eggs. Robotic egg fertilization eliminates human tremor and fatigue factors that can compromise success rates. Automated sperm selection removes subjective bias, while remote-operated capabilities allow specialists to oversee procedures from different locations.
This technological integration addresses longstanding challenges in reproductive medicine, including inconsistent outcomes due to human variability and limited access to specialized expertise. The system’s ability to operate with minimal direct human intervention while maintaining safety protocols represents a significant advancement in medical automation.
https://www.youtube.com/watch?v=UqIEyOuB3XQ
Performance Comparison: Robots vs. Human Embryologists
The comparison between automated robotic systems and human embryologists reveals fascinating differences in speed, consistency, and outcomes. Recent data shows that manual ICSI performed by skilled embryologists required an average of 1 minute and 22 seconds per egg, with all 3 processed eggs achieving successful fertilization – a perfect success rate that demonstrates the expertise of trained professionals.
Speed and Efficiency Metrics
Automated robotic systems currently operate at a different pace, taking an average of 9 minutes and 56 seconds per egg during testing phases. This represents roughly seven times longer than human operators, but the context matters significantly. Artificial intelligence systems typically require extended processing time during initial implementations as they execute precise protocols without shortcuts that experienced humans naturally develop.
The robotic system processed 5 eggs during trials, achieving fertilization in 4 out of 5 attempts. This 80% success rate, while slightly lower than the human benchmark, falls within acceptable clinical parameters for IVF procedures. More importantly, the automated approach delivered consistent results across multiple attempts, suggesting reduced variability that often affects human performance due to fatigue or environmental factors.
Consistency and Future Optimization
The key advantage of robotic systems lies in their unwavering consistency. While human embryologists might experience performance fluctuations throughout long procedures, robotic technology maintains identical precision levels regardless of duration or complexity. This consistency becomes particularly valuable during extended laboratory sessions where multiple procedures occur simultaneously.
Optimization potential represents perhaps the most compelling aspect of these early results. Unlike human capabilities that improve gradually through experience, robotic systems can receive software updates that instantly enhance performance across all units. Engineers anticipate significant speed improvements as algorithms become more refined and hardware components are optimized for specific tasks.
Current data suggests that robots excel in maintaining sterile environments and executing micro-movements with mathematical precision. Human embryologists still demonstrate superior adaptability and problem-solving capabilities when unexpected situations arise. However, AI technology advancement continues to bridge these gaps through machine learning algorithms that improve decision-making processes.
The promising performance metrics indicate that automated systems could complement rather than replace human expertise, potentially handling routine procedures while embryologists focus on complex cases requiring specialized judgment and intervention strategies.
Why Scientists Are Automating IVF and Its Medical Benefits
Automation in fertility treatments represents a significant advancement in reproductive medicine, driven by the need to address long-standing challenges in traditional IVF procedures. Scientists have recognized that human error and variability pose substantial risks during delicate embryo manipulation processes, potentially leading to egg degeneration or fertilization failure that can devastate couples hoping to conceive.
Standardization and Precision Advantages
Robotic systems deliver consistent performance that eliminates the variability inherent in manual procedures. Even the most skilled embryologists can experience fatigue during long procedures, which directly impacts their precision and decision-making abilities. Automated systems maintain the same level of accuracy throughout extended operations, ensuring that each egg receives identical treatment regardless of the time of day or duration of the procedure.
The gentle nature of artificial intelligence guided operations significantly reduces mechanical stress on delicate egg cells. Traditional manual manipulation requires physical handling that can inadvertently damage these fragile structures, but robotic precision minimizes this risk through carefully calibrated movements and pressure application.
ICSI technology, which originated in the 1990s, involves injecting a single sperm directly into an egg and has become essential for addressing male infertility issues. This procedure requires extraordinary precision that benefits tremendously from automation. Robotic systems can position the injection needle with microscopic accuracy, ensuring optimal sperm placement while minimizing cellular trauma.
The scalability benefits of automation address a growing global demand for fertility services. Traditional IVF clinics face limitations in the number of procedures they can perform due to the specialized skill requirements and time-intensive nature of manual processes. Robotic systems can operate continuously and handle multiple procedures simultaneously, dramatically increasing clinic capacity.
Economic and Clinical Benefits
Cost reduction represents another compelling advantage of automated IVF processes. While initial equipment investments are substantial, the long-term economics favor automation through reduced labor costs and improved success rates. These savings can eventually translate into more affordable treatments for patients, making fertility services accessible to couples who previously couldn’t afford multiple IVF cycles.
Improved egg survival rates directly correlate with better pregnancy outcomes. Automated systems apply consistent pressure and temperature control during egg manipulation, factors that critically influence cellular viability. Manual procedures often introduce temperature fluctuations and varying pressure levels that can compromise egg quality, whereas robotic systems maintain optimal conditions throughout the entire process.
The reduction of human error extends beyond simple mistakes to include the elimination of subjective decision-making that can vary between practitioners. Automated systems follow predetermined protocols based on optimal parameters, ensuring that each embryo receives treatment according to the highest standards rather than individual practitioner preferences or experience levels.
Enhancing Global Access and Quality Control
Quality control becomes more achievable through automation since every procedure can be monitored, recorded, and analyzed for continuous improvement. This data collection capability allows scientists to refine techniques and identify optimal conditions for different patient populations, something that’s difficult to achieve with manual procedures where variables are harder to control and measure.
Accessibility improvements through automation could revolutionize fertility treatment availability in underserved areas. Regions lacking specialized embryologists could potentially offer IVF services with robotic assistance, reducing the geographic barriers that currently prevent many couples from accessing treatment. Advanced technology integration makes it possible to provide consistent, high-quality care regardless of location.
The integration of machine learning capabilities allows automated systems to continuously improve their performance based on accumulated data from thousands of procedures. These systems can identify patterns and optimize protocols in ways that individual practitioners might not recognize, leading to progressively better outcomes over time.
https://www.youtube.com/watch?v=ZxdUe4qNFRA
What This Means for the Future of Fertility Treatment
This groundbreaking achievement establishes a working model for standardized, precise, and scalable embryo creation through automation. I see this development as a potential game-changer that could fundamentally reshape how fertility clinics operate worldwide. The technology demonstrates that artificial intelligence paving the way extends far beyond traditional applications into the deeply personal sphere of human reproduction.
The Vision for Complete Automation
The long-term vision encompasses complete automation—from fertilization to embryo selection—with ongoing human supervision for each treatment cycle. This approach promises to transform IVF laboratories from manually intensive environments into highly controlled, precise operations. Advanced robotics could handle delicate procedures with consistency that human hands simply can’t match, reducing variability between cycles and potentially improving success rates.
As the technology improves, it carries the potential to streamline IVF procedures, cut costs significantly, and make assisted reproduction services more accessible to couples who previously couldn’t afford treatment. Lower costs could democratize fertility care, bringing hope to thousands of families currently priced out of these essential services.
Expert Perspectives and Cautious Optimism
Experts such as Dr. Erkan Buyuk and Dr. Emily Jungheim recognize the importance of this breakthrough but caution that comprehensive research and validation remain necessary to ensure safety and efficacy. Their measured response reflects the medical community’s responsibility to balance innovation with patient safety. I believe their cautious approach is warranted given the profound implications of automating human reproduction.
While the robotic system has potential to transform laboratory workflows in IVF, the role of embryologists will remain essential for monitoring, safety, and troubleshooting. These professionals won’t become obsolete; instead, their roles will evolve to focus on oversight, quality control, and managing complex cases that require human judgment.
This technology could standardize procedures across different clinics, potentially reducing the wide variation in success rates that currently exists between facilities. Imagine a future where AI-driven systems ensure consistent, optimal conditions for every embryo, regardless of which clinic provides the treatment. The implications extend beyond individual success stories to broader healthcare equity and access to reproductive care.

Sources:
Conceivable Life Sciences
Reproductive BioMedicine Online
Mount Sinai/RMA of New York
Northwestern Medicine


