Japan’s revolutionary tooth regrowth medication has entered human trials, marking a historic breakthrough that could transform dental care by permanently eliminating the need for dentures and implants.
Key Takeaways
- Human trials are underway – Thirty healthy adult males aged 30-64 with missing teeth are participating in Phase 1 trials through August 2025. A second phase will test children born with congenital tooth absence.
- The medication works by blocking USAG-1 – This protein naturally inhibits tooth growth. Blocking it reactivates dormant tooth buds to grow a third set of natural, fully functional teeth.
- Animal studies show complete success – Trials on mice and ferrets demonstrated that the treatment produces healthy, structured teeth that integrate naturally with jawbone and gums.
- Massive global impact potential – While initially targeting the 1% of people born with congenital tooth deficiency, this treatment may eventually help millions who’ve lost teeth to decay, disease, or injury.
- Superior to current solutions – Unlike implants or dentures that require replacement over time, regenerated natural teeth could last a lifetime with proper care.
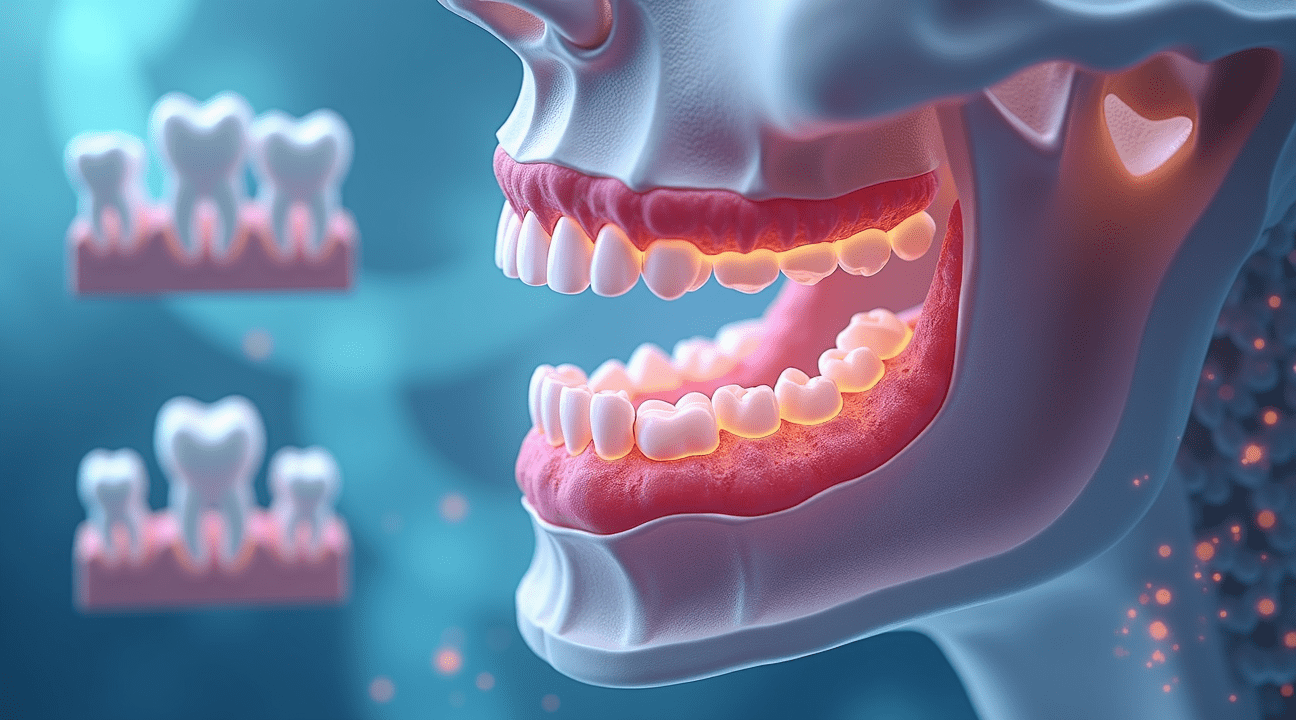
The Science Behind Tooth Regeneration
The scientific breakthrough centers on the discovery that USAG-1, a specific protein, acts as a natural brake on tooth development. Researchers found that blocking this protein reactivates dormant tooth buds hidden within the jaw bone. Once reactivated, these buds can form complete and functional teeth.
Animal Trials Show Promise
Animal testing has shown highly impressive results. Mice were able to regrow perfectly structured and fully functional teeth. Further testing on ferrets confirmed the treatment’s viability in mammals whose dental structures closely resemble humans. The regenerated teeth showed proper enamel layers, root development, and nerve integration.
Current Progress in Human Trials
The current human trials are primarily focused on evaluating safety. Thirty adult males with missing molars are receiving meticulously controlled doses of the USAG-1-blocking drug. Doctors are monitoring participants for any adverse reactions while observing early signs of tooth bud activation. This phase will continue until August 2025 and will provide essential data on dosage levels and treatment timelines.
Future Phases and Populations
Should Phase 1 succeed, researchers will begin trials on children born with congenital absence of permanent teeth. This condition affects around 1% of all births and poses lifelong dental challenges. Current solutions provide only partial relief. Natural tooth regeneration could become the first true permanent fix.
Broad Global Applications
While the current target group involves congenital conditions, the broader implications of this research include treatment for billions affected by tooth loss from decay, trauma, or disease. Conventional treatments like implants and dentures come with drawbacks—cost, discomfort, and eventual failure. Natural tooth regrowth could eliminate these issues entirely.
Economic and Healthcare Impact
The potential economic benefits of this technology are immense. Implant procedures often cost thousands per tooth and require surgical expertise, making access difficult for many patients. Tooth regeneration could become a one-time, lower-cost option. With permanent results, it may also make insurance approval more likely.
Challenges and Considerations
Despite its promise, the path forward includes several scientific and technical challenges:
- Precisely timing treatment to align with each individual’s jaw development.
- Refining dosage to activate only desired tooth buds, avoiding possible overgrowth.
- Monitoring integration with existing teeth and ensuring bite alignment.
Moreover, the process must replicate the complex genetic programming involved in natural tooth formation. Ensuring consistent root strength, crown structure, and nerve development is essential for widespread application.
Timeline and Worldwide Collaboration
The 2030 release target reflects the extensive testing and validation needed. Future phases will explore efficacy across different ages and tooth types. Regulatory agencies will evaluate long-term safety and determine how this innovation can be incorporated into clinical dental practice.
Global interest is growing steadily. Worldwide research teams are closely watching the Japanese trials. Collaboration could accelerate the accumulation of data and streamline the approval process, potentially shortening timelines across borders.
Planning for Widespread Use
Production and distribution planning are already underway. Manufacturing the drug will require specialized facilities with tight quality control. Dental professionals will need certification programs to safely administer the treatment.
Future Patient Eligibility
Initially, treatment will cater to narrow patient profiles—those with healthy gums, strong bone structure, and realistic expectations. Broader eligibility will depend on accumulating safety data from ongoing studies.
A Turning Point in Dental Science
This innovation is the product of decades of fundamental research into how teeth form, how dormant tooth buds operate, and how protein signals affect growth. The work of Dr. Katsu Takahashi and his team stands as a milestone in regenerative medicine.
If their human trials prove successful, Japan’s tooth regrowth medication could revolutionize dentistry within a generation. Natural tooth regeneration has the potential to make dentures and implants obsolete and could introduce a new era in oral healthcare.
Revolutionary Tooth Regrowth Drug Enters Human Trials in Japan
Groundbreaking human trials for a tooth regrowth medication have officially commenced in Japan, marking a significant milestone in dental science. Dr. Katsu Takahashi and his research team at Kitano Hospital and Kyoto University Hospital launched these clinical trials in September and October 2024, representing the culmination of years of laboratory research.
First Phase Testing with Adult Participants
The initial phase of this clinical trial involves 30 healthy adult males, carefully selected within the age range of 30 to 64 years. Each participant shares a common characteristic: the absence of at least one tooth. This selective criteria allows researchers to precisely evaluate the drug’s effectiveness in stimulating tooth regrowth in real-world conditions. The trial will continue through August 2025, providing researchers with nearly a full year of data collection and safety monitoring.
During this extended period, the team is expected to closely monitor participants for any adverse reactions while documenting the drug’s ability to trigger natural tooth regeneration. Safety remains the primary concern during this phase, as researchers must establish that the medication presents minimal risk before advancing to subsequent trials.
Children’s Phase and Future Availability
Following successful completion of the adult safety phase, the second phase will focus on children aged 2 to 7 who suffer from congenital tooth absence conditions. These young participants will have anodontia or oligodontia, conditions where individuals are missing four or more teeth from birth. This phase holds particular significance because it addresses a vulnerable population that currently faces limited treatment options.
The research team has established an ambitious timeline for bringing this revolutionary treatment to the general public by 2030. This target date reflects their confidence in the drug’s potential while acknowledging the rigorous testing required for such an innovative treatment. Children with congenital tooth absence often struggle with eating, speaking, and social confidence, making this research particularly meaningful for families affected by these conditions.
Current dental solutions like robotic prosthetics and implants may become obsolete if this medication proves successful. The implications extend beyond individual patient care to potentially transforming the entire dental industry. Unlike traditional prosthetics that require replacement and maintenance, naturally regrown teeth would integrate seamlessly with existing oral structures.
Dr. Takahashi’s team has spent years perfecting this approach, which targets specific proteins responsible for tooth development. Their research builds upon understanding how teeth naturally form during human development, essentially reactivating dormant biological processes. This scientific breakthrough could eliminate the need for dentures and implants forever, offering patients authentic tooth replacement rather than artificial substitutes.
How the Medication Works to Regenerate a Third Set of Teeth
The groundbreaking medication operates through a sophisticated biological mechanism that targets USAG-1, a protein that serves as a natural tooth growth inhibitor in the human body. I find this approach particularly fascinating because it essentially hijacks the body’s existing biological pathways rather than introducing foreign substances to force tooth development.
USAG-1 acts as a biological brake system, preventing dormant tooth buds from activating throughout a person’s lifetime. These tooth buds exist naturally in human jaws but remain inactive due to this protein’s suppressive effects. When researchers discovered they could block USAG-1’s inhibitory function, they unlocked the potential for humans to develop what scientists call a third set of teeth — a capability that mirrors certain animals’ natural regenerative abilities.
Animal Study Results Provide Proof of Concept
The medication’s effectiveness has been demonstrated through extensive animal studies involving mice and ferrets. These trials revealed several key findings that support the treatment’s viability:
- Complete blockage of USAG-1 successfully triggered dormant tooth buds to activate and begin growing
- The newly formed teeth developed normal structure and functionality, matching the quality of natural teeth
- Test subjects showed no adverse effects from the protein-blocking treatment
- The regenerated teeth integrated properly with existing jaw bone and gum tissue
Ferrets proved particularly valuable as test subjects because their dental development closely mirrors human tooth formation patterns. When researchers administered the USAG-1-blocking medication to these animals, they observed healthy, functional teeth emerging from previously inactive tooth buds. This mirrors what happens in sharks and other animals that naturally regenerate teeth throughout their lives, though humans typically only develop two sets — baby teeth and permanent teeth.
The technical breakthrough lies in understanding that humans actually possess the genetic blueprint for continuous tooth regeneration. USAG-1 simply prevents this natural capability from expressing itself after permanent teeth emerge. By temporarily suppressing this protein’s activity, the medication essentially turns the body into a liquid-like state of regenerative potential, allowing dormant biological systems to reactivate.
Mouse studies provided additional confirmation that blocking tooth growth inhibitors produces reliable results across different mammalian species. Researchers noted that the newly grown teeth developed proper enamel, dentin, and root structures without requiring additional interventions or supportive treatments.
The medication’s precision targeting represents a significant advancement over previous regenerative approaches that often produced incomplete or malformed dental structures. Instead of attempting to grow teeth from scratch using stem cells or scaffolding materials, this treatment activates the body’s existing capacity for tooth development.
Scientists believe this biological pathway remains intact in adult humans despite decades of inactivity. The dormant tooth buds contain all necessary cellular machinery to produce fully functional teeth when properly stimulated through USAG-1 suppression.
Current research focuses on determining optimal dosing protocols and treatment duration for human applications. Animal studies suggest that temporary inhibition of USAG-1 provides sufficient stimulus for complete tooth development, after which the protein’s natural function can resume without interfering with the newly formed dental structures.
The regenerated teeth demonstrate remarkable similarity to natural permanent teeth in terms of hardness, appearance, and functional capacity. This outcome addresses concerns about whether artificially triggered tooth development could produce inferior dental structures compared to conventional implants or dentures.
Understanding how essential building blocks interact within biological systems helps explain why this protein-blocking approach succeeds where other regenerative techniques have struggled. The medication works with existing biological processes rather than against them, resulting in more predictable and successful outcomes.
Who Could Benefit and the Massive Scale of Impact
The groundbreaking tooth regrowth medication initially targets patients with congenital tooth deficiency, a condition that affects approximately 1% of the global population. I find it remarkable that this seemingly small percentage translates to millions of individuals worldwide who could finally have a permanent solution to their dental challenges.
Primary Beneficiaries and Current Focus
Severe cases involving oligodontia, where patients have more than six missing teeth, affect about 0.1% of the population. In Japan alone, this represents roughly 120,000 individuals living with significant dental deficiencies. These patients currently rely on:
- Complex dental procedures
- Multiple implants
- Extensive denture systems that require frequent adjustments and replacements
The medication offers hope for those with anodontia as well, a rare condition where individuals are born without tooth buds. Traditional treatments for these patients involve:
- Years of surgical procedures
- Early and ongoing prosthetic management
I believe this revolutionary approach could transform their entire dental experience from artificial replacements to natural, living teeth.
Expanding Applications and Global Reach
Developers have ambitious plans to extend the medication’s applications beyond congenital conditions. Future iterations aim to help individuals who have lost teeth due to:
- Decay
- Accidents
- Disease
These conditions affect millions worldwide and this expansion could revolutionize dental care on a scale similar to how antibiotics changed medicine.
The global impact becomes staggering when considering tooth loss statistics. Causes include:
- Dental trauma from accidents
- Tooth decay, one of the most prevalent global diseases
- Aging populations in developed countries
This medication could address all these scenarios with a single, natural approach to dental restoration.
The benefits go beyond simple tooth replacement. Natural, living tooth regrowth offers advantages artificial alternatives cannot match:
- Seamless integration with existing oral structures
- Proper blood flow and nerve connections for enhanced sensation and function
Much like how innovative technologies are transforming various fields, this medical breakthrough could reshape dental care entirely.
Patients could experience dramatically lower lifetime dental costs, due to long-lasting results. Traditional solutions come with repeat expenses:
- Implants require replacement every 10–20 years
- Dentures need frequent adjustments and eventual replacement
Regrown teeth, being natural biological structures, could potentially last a lifetime with proper care, eliminating the cycle of expensive dental procedures many endure.
Quality of life improvements represent perhaps the most significant benefit:
- Better chewing ability improves nutrition and digestion
- Improved speech capabilities enhance communication and career opportunities
- Confidence from natural-looking teeth boosts social and mental well-being
The medication’s development parallels other scientific breakthroughs that seemed impossible just decades ago. Scientific discoveries continue to push boundaries, and tooth regeneration represents another frontier in medical science.
Early candidates for treatment include:
- Children with congenital deficiencies, benefiting from early intervention
- Adults who’ve lost teeth due to trauma or disease, regaining full function naturally
The ripple effects could transform the entire dental industry:
- Reduced demand for implants, dentures, and related procedures
- Increased focus on preventive care and regenerative treatments
- New training protocols for dental professionals
This medication represents more than just another dental treatment option—it offers the possibility of returning patients to their natural state instead of managing their condition artificially. The potential impact spans from individual quality of life improvements to industry-wide transformations in dental care practices.
How This Compares to Dental Implants and Dentures
The groundbreaking tooth regeneration medication represents a fundamental shift from current dental restoration methods. Unlike the titanium or ceramic artificial roots used in dental implants, this treatment works with natural biological tissues to regrow actual teeth. Traditional dentures rely on acrylic or plastic materials, while this innovative approach stimulates the body’s own tooth development processes.
Longevity and Durability Differences
Natural teeth potentially offer decades of service, far exceeding the typical lifespan of conventional treatments. Dental implants generally last 10–30 years before requiring replacement, while dentures need updating every 5–10 years due to wear and changes in jaw structure. The regenerated teeth, being genuine living tissue, could theoretically last a lifetime with proper care, similar to how advanced technologies are reshaping various fields of medicine and science.
Treatment Methods and Integration
The delivery method for this medication involves IV drug administration, with researchers hoping to develop oral formulations in the future. This contrasts sharply with the surgical placement required for implants, which involves drilling into the jawbone to anchor artificial roots. Dentures require only non-surgical fitting and adjustment processes.
Natural regrowth provides fully integrated living tissue that connects seamlessly with existing jawbone structure.
- Dental implants offer osseointegration, where bone grows around the titanium post, but the implant itself remains non-living material.
- Dentures have no biological integration whatsoever, simply resting on the gums and relying on suction and adhesives for stability.
Maintenance requirements also differ significantly:
- Regenerated teeth require the same care as natural teeth – regular brushing, flossing, and dental checkups.
- Implants need special cleaning protocols and frequent professional monitoring to prevent complications like peri-implantitis.
- Dentures demand daily removal for cleaning, special solutions, and frequent adjustments as the mouth changes shape over time.
The target demographic varies considerably between treatments:
- This medication initially focuses on all age groups, particularly those with congenital tooth absence.
- Current dental implants and dentures primarily serve adults and elderly patients who’ve lost teeth through decay, injury, or disease.
The regenerative approach could potentially eliminate the need for prosthetic solutions entirely, offering patients genuine biological replacements rather than artificial substitutes.
Safety Research and What Scientists Are Monitoring
Animal testing showed promising results with minimal complications, setting the stage for human evaluations. I’ve followed these developments closely, and researchers are taking an extremely cautious approach with their first-in-human trials. The team prioritizes safety confirmation before measuring how effectively the drug regenerates teeth.
Primary Safety Monitoring Parameters
Scientists track several critical factors during these trials. The research team monitors dose responses carefully, determining the optimal amount of USAG-1 antibody needed for tooth regeneration without triggering adverse reactions. They’re documenting every side effect, no matter how minor, creating a comprehensive safety profile.
Adverse event monitoring extends beyond immediate reactions. Researchers examine participants for weeks and months after treatment, watching for delayed complications that might not appear immediately. This extended observation period helps identify potential long-term health impacts that animal studies couldn’t predict.
While other innovative approaches like robotic technology continue advancing various medical fields, dental regeneration remains focused on biological solutions. The integration process between newly grown teeth and existing oral structures receives intense scrutiny. Scientists evaluate how well regenerated teeth bond with gum tissues and align with jaw structures.
Long-term Durability and Functionality Assessment
The functionality of regrown teeth presents unique challenges that researchers must address. I’ve learned that scientists assess bite strength, chewing efficiency, and overall tooth durability compared to natural teeth. They’re particularly interested in whether these regenerated teeth can withstand normal eating patterns and maintain their strength over years of use.
Integration with surrounding tissues requires detailed analysis. Researchers examine how the new teeth connect with existing bone structures and whether they develop proper root systems. Blood vessel formation around the new teeth is another crucial factor, as adequate circulation ensures long-term tooth health.
The nerve development within regenerated teeth presents another monitoring challenge. Scientists track whether these teeth develop proper sensation and pain responses, which are essential for normal oral function and protection against damage.
Other regenerative approaches, including stem cell-based tooth regeneration, remain in earlier research phases. These alternative methods show promise but haven’t reached human testing stages yet. The USAG-1 antibody drug represents the first regenerative dental treatment to advance to human trials, making its safety profile particularly valuable for future developments.
Researchers also monitor participants’ overall oral health throughout the trial period. They track changes in gum health, tooth alignment, and bite patterns that might result from new tooth growth. This comprehensive approach ensures that regenerating teeth doesn’t negatively impact existing dental structures.
The psychological impact on participants receives attention as well. Scientists document how the experience of tooth regeneration affects patients’ confidence and quality of life. This data helps researchers understand the broader implications of successful tooth regeneration beyond purely medical outcomes.
Long-term follow-up studies will continue for years after initial treatment. I expect these extended monitoring periods will provide crucial data about the permanent viability of regenerated teeth. Scientists plan to track participants for at least five years, with some studies potentially extending much longer.
The success of these safety evaluations will determine whether this groundbreaking treatment moves forward to larger clinical trials. Current results suggest that the USAG-1 antibody approach maintains an acceptable safety profile, but researchers continue gathering comprehensive data to ensure patient protection. The careful monitoring protocols established in these early trials will likely influence how future dental regeneration treatments are evaluated and implemented.
The End of Dentures and Artificial Implants Era
I’ve witnessed countless dental innovations throughout history, but none have carried the revolutionary potential of Japan’s groundbreaking tooth regrowth medication. This development represents far more than a simple advancement in dental technology—it signals a complete paradigm shift that could permanently alter how we approach missing teeth.
A Global Impact on Dental Practice
The implications of successful tooth regeneration extend far beyond Japan’s borders. Dental professionals worldwide are closely monitoring these trials, recognizing that this breakthrough could fundamentally transform their practice models. Traditional dental care has long relied on artificial solutions, from basic dentures to sophisticated titanium implants, but the possibility of regrowing natural teeth challenges these established methods.
The end of dentures represents a particularly significant milestone for millions of people who currently struggle with the limitations of removable prosthetics. Unlike dentures that often slip, require adhesives, and limit food choices, regenerated teeth would function exactly like natural ones. I find it fascinating how technology continues to push boundaries, much like how robots escape cages using innovative approaches.
Economic ramifications could be substantial. The global dental implant market, currently valued in billions of dollars, might face significant disruption if tooth regeneration becomes commercially viable. Dental laboratories that specialize in creating artificial teeth, crown manufacturers, and implant companies would need to adapt their business models or risk obsolescence.
Dental Care Transformation Beyond Replacement
The Japanese medication doesn’t just offer an alternative to current tooth replacement methods—it represents a complete rethinking of dental care philosophy. Instead of accepting tooth loss as inevitable and focusing on artificial replacements, dental professionals could shift their approach toward regenerative solutions.
This transformation extends to patient psychology and quality of life considerations. Artificial implants, while effective, require surgery, healing time, and ongoing maintenance. The psychological comfort of having one’s own regenerated teeth versus artificial alternatives could prove invaluable for patient confidence and oral health outcomes.
The medication’s success could also influence research directions in other medical fields. Regenerative medicine has shown promise in various applications, from organ replacement to wound healing. The principles behind tooth regrowth might find applications in bone regeneration, cartilage repair, or other tissue restoration projects.
Prevention strategies might evolve as well. If teeth can be regrown reliably, dental professionals might approach treatment differently, potentially being more aggressive in removing severely damaged teeth rather than attempting complex preservation procedures. This shift could streamline treatment protocols and improve patient outcomes.
The dental revolution I’m observing represents something unprecedented in modern medicine. While scientists have made remarkable discoveries in space, such as finding life building blocks on Saturn’s moon, the prospect of regrowing human teeth brings science fiction into everyday reality.
Training and education systems for dental professionals would require complete overhaul. Dental schools would need to incorporate regenerative medicine principles into their curricula, while practicing dentists would need continuing education to understand and implement these new treatments.
The ripple effects could influence insurance coverage policies, treatment costs, and accessibility to dental care. If tooth regeneration proves more cost-effective than implants over time, insurance companies might prefer covering the medication over expensive surgical procedures.
International collaboration in dental research could accelerate dramatically. Countries with advanced biotechnology sectors might rush to develop their own versions of regenerative dental treatments, leading to faster innovation cycles and potentially more affordable options for patients worldwide.
The end of the dentures and artificial implants era isn’t just about replacing old technology with new—it’s about fundamentally changing how humans maintain their oral health throughout their lives. This Japanese innovation could usher in an age where losing teeth doesn’t mean permanent loss, but rather temporary inconvenience before regeneration.
Sources:
Mainichi
Tasnim News – “Scientists Begin Human Trials for Tooth-Regrowing Drug”
Dentistry.co.uk – “Tooth Regrowth in Adults: What We Know So Far”
Dentistry Today – “Researchers in Japan Discover Medicine Capable of Regrowing Third Set of Teeth for Humans”
Luminance Dentaire – “Japan Begins Human Trials for Tooth Regrowth Drug TRG-035”
Dentinova – “Dr. Katsu Takahashi Latest News About Tooth Regrowth Drug”
Concierge Dental Group – “Japanese Scientists Begin Human Trials for Tooth Regrowth Drug”
Crown and Denture – “Tooth Regrowth Drug in Japan: Future of Dental Care”


