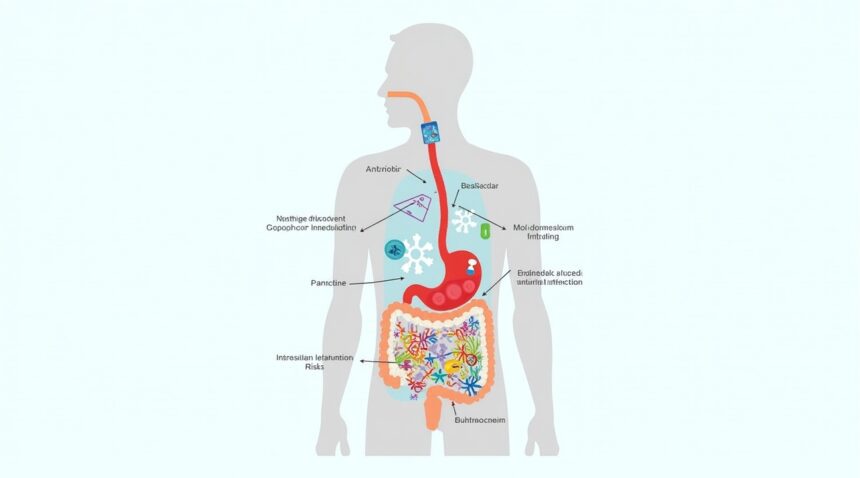
Recent research reveals that 93 out of 186 commonly prescribed medications cause lasting changes to the gut bacteria composition—alterations that can persist for years after patients cease taking the drugs.
Key Takeaways
- Nearly half of common medications cause long-lasting gut bacteria changes – 93 out of 186 studied drugs cause microbiome alterations that persist years after treatment ends.
- Five major drug categories show the strongest impact – Antibiotics, beta-blockers, benzodiazepines, proton-pump inhibitors, and antidepressants all leave long-lasting bacterial imprints.
- Multiple medications compound the effects – Patients on several drugs, or undergoing repeated treatments, exhibit greater and more persistent microbiome disruptions.
- Even non-digestive medications reshape gut bacteria – Medications for heart conditions, anxiety, and depression significantly alter the intestinal microbiome via direct and indirect pathways.
- Healthcare providers must track medication history – Past pharmaceutical use critically shapes current microbiome profiles, highlighting the need for thorough medication documentation.
Understanding the Scope of Pharmaceutical Impact on Gut Health
The scale of pharmaceutical impact on gut bacteria is more extensive than previously assumed. Scientists analyzed data across diverse patient populations and medication regimens and found that even drugs not typically considered digestive influencers caused measurable changes in the gut microbiome.
While antibiotics were expected to top the list, the research revealed surprising disruptors. Beta-blockers prescribed for hypertension, benzodiazepines for anxiety, and proton-pump inhibitors (PPIs) for acid reflux all modified bacterial communities. These effects were not only immediate but often persisted well beyond the end of treatment.
The Five Major Drug Categories Creating Lasting Change
Antibiotics: The Primary Disruptors
Antibiotics severely disrupt gut microbiota, wiping out both harmful and beneficial strains. Research shows that:
- Broad-spectrum antibiotics, like fluoroquinolones and macrolides, produce the most severe damage.
- Microbial diversity can take years to recover, with some strains never returning.
- Even short antibiotic courses leave microbial changes detectable 3–5 years later.
Beta-Blockers: Unexpected Gut Modifiers
Beta-blockers alter gut bacteria through changes in gut motility and blood flow. Key observations include:
- Propranolol and metoprolol exhibit the most pronounced microbiome modifications.
- Long-term users develop consistent microbial signatures affecting digestion and inflammation.
- Changes are especially seen in bacteria involved in producing vital short-chain fatty acids.
Benzodiazepines: Anxiety Medications That Reshape Bacteria
Through the gut-brain axis, benzodiazepines impact bacteria by influencing neurotransmitters and immune responses.
- Lorazepam and diazepam significantly reduce microbiota diversity with use duration.
- These effects can outlast usage for months or even years.
- Altered gut motility and immune reaction contribute to sustained changes.
Proton-Pump Inhibitors: Acid Suppression with Bacterial Consequences
PPIs lower stomach acidity, disrupting the gut ecosystem in several ways:
- Omeprazole and esomeprazole increase harmful bacteria like Enterococcus and Streptococcus.
- Beneficial, acid-dependent strains decline significantly.
- These bacterial shifts remain present years after stopping therapy.
Antidepressants: Mental Health Medications with Gut Effects
SSRIs such as sertraline and fluoxetine modify gut flora by altering neurotransmitters, gut movement, and immune signaling.
- SSRI usage alters bacteria associated with GABA and serotonin production.
- The resulting microbial profiles often persist after treatment cessation.
- Some changes may influence mood and immune responses long term.
Mechanisms Behind Persistent Bacterial Changes
Several factors contribute to why these changes endure post-treatment:
- Gut environmental changes – Medications modify pH, motility, and mucosal conditions, favoring certain bacteria.
- Direct drug-bacteria interactions – Drugs can feed, suppress, or kill specific bacterial types based on chemical structure.
- Immune modulation – Medications influence cytokine production and immune cell activity, cementing new microbial balances.
Compounding Effects of Multiple Medications
Polypharmacy poses a greater risk for microbiota disruption:
- Drug combinations such as PPIs with antibiotics cause extensive microbiota damage.
- Sequential or long-term regimens create accumulated changes that limit microbial resilience.
- Microbiome alterations become compounded, making recovery increasingly difficult.
Clinical Implications for Healthcare Practice
Medical professionals need to reconsider prescription strategies and microbiome management practices:
- Obtain detailed medication histories for the last 5 years to understand gut-related symptoms.
- Customize treatment plans that factor in past prescriptions and bacterial impacts.
- Stagger prescriptions of gut-altering drugs to allow microbial recovery.
Strategies for Minimizing Long-Term Bacterial Damage
Prevention strategies can mitigate the lasting effects of medications:
- Probiotic supplements support microbiome stability during and after treatment.
- Prebiotic-rich diets — such as those with fiber, garlic, and onions — nourish beneficial bacteria.
- Fermented foods introduce diverse strains and aid recovery post-medication.
- Thoughtful drug selection within medication classes can minimize microbial disruption.
Future Research Directions and Clinical Applications
Ongoing studies aim to understand the broader health implications of these microbiome changes. Early findings indicate links to increased risks of:
- Infections
- Autoimmune disorders
- Metabolic syndrome
Emerging approaches include:
- Personalized medicine – Pre-treatment profiling of gut bacteria may guide safer drug choices.
- Drug development – Future formulations could reduce gut bacterial damage or bypass the gut entirely.
- Genetic testing – May help predict individual susceptibility to microbiome disruption.
This groundbreaking research transforms how we understand the relationship between medication and long-term gut health. The assumption that drug effects cease with treatment no longer applies to the microbiome. To improve outcomes, healthcare providers must now consider every prescription as a potential long-term modifier of a patient’s bacterial ecosystem.
Nearly Half of Common Drugs Cause Years-Long Changes to Your Gut Bacteria
Recent research reveals that 93 out of 186 commonly prescribed medications create lasting changes to gut bacteria composition that persist for years after patients stop taking them. This discovery fundamentally challenges the assumption that medication effects on the microbiome are temporary and reversible.
Multiple Drug Classes Create Persistent Microbiome Disruption
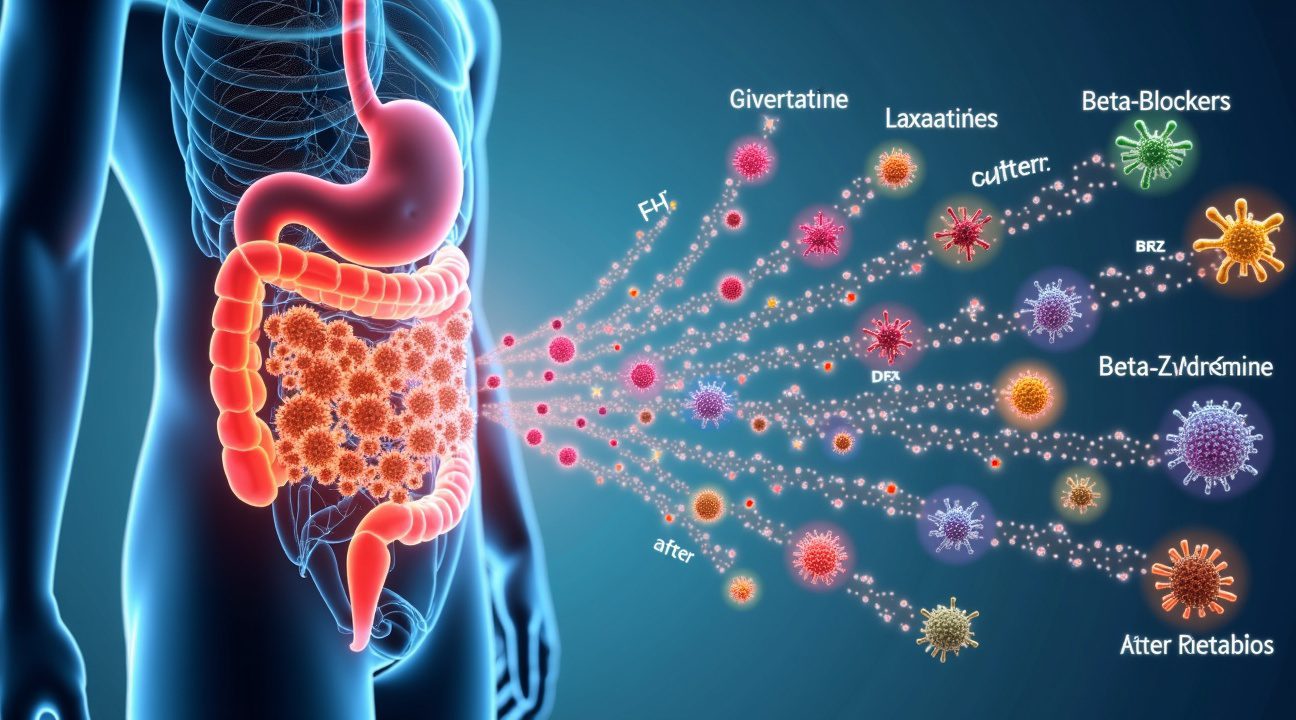
Five major categories of medications demonstrate particularly strong associations with long-term gut bacteria alterations:
- Antibiotics – unsurprisingly top the list due to their broad-spectrum bacterial killing mechanisms.
- Beta-blockers – commonly prescribed for heart conditions and high blood pressure, significantly modify microbial communities long beyond treatment.
- Benzodiazepines – used for anxiety and sleep disorders, create distinct changes in gut bacteria diversity.
- Proton-pump inhibitors (PPIs) – used to treat acid reflux and stomach ulcers, alter the stomach’s pH balance, affecting bacterial viability in the gut.
- Antidepressants – medications affecting brain chemistry also reshape the gut-brain axis at the microbial level.
Cumulative Effects Amplify Microbiome Disruption
The impact becomes more pronounced when patients take multiple medications or undergo repeated treatment courses. Each additional drug or treatment cycle compounds the effects on gut bacteria diversity and composition. Patients with complex medication regimens often show the most dramatic shifts in their microbial profiles.
These cumulative effects do not add together in a simple linear fashion. Instead, they create complex interactions in which one medication can amplify or alter how another drug affects the gut microbiome. For example, a patient taking both a PPI and an antibiotic may experience more extensive microbiome changes than someone taking just one of those medications.
The persistence of these changes varies based on the specific medication and individual factors. Some bacterial populations never fully regain their original diversity levels, even years later. In other cases, certain species may return, but the overall gut community structure becomes permanently altered. This leads to a new “normal” gut state that differs markedly from the pre-treatment condition.
Healthcare providers and researchers must now consider medication history as a critical factor when evaluating microbiome-related health outcomes. A patient’s current gut bacteria profile may reflect not only recent medication but also the cumulative impact of years—even decades—of pharmaceutical use. This insight has profound implications for personalized medicine approaches that utilize microbiome analysis.
The findings also highlight the importance of timing between treatments. Starting a new drug while the gut is still recovering from a previous one may prevent full restoration of bacterial diversity. Strategically spacing medications could help minimize microbiome disruption, although this must be balanced carefully with the patient’s immediate therapeutic needs.
Understanding these long-lasting effects opens new avenues for treatment optimization. Clinicians can now factor in potential microbiome consequences when weighing medication choices, particularly for chronic conditions requiring long-term treatment. Medications with biological impact clearly extend far beyond their primary therapeutic targets.
The research underscores the need for proactive microbiome support during and after medication use. Strategies such as probiotic supplementation, dietary changes, and other microbiome-focused interventions may help counteract some long-term effects. However, the complexity of drug-microbe interactions suggests that uniform solutions are unlikely to work for everyone.
Going forward, drug development must include microbiome impact assessment as a standard part of the evaluation process. The bacterial shifts uncovered in this research represent a previously underappreciated category of side effects—one that warrants the same level of scrutiny as more traditional adverse reactions. This paradigm shift could transform how pharmaceutical treatments are designed and how long-term care is managed.
Antibiotics Kill Good Bacteria Along With the Bad – And the Damage Lasts
Antibiotics don’t discriminate between harmful pathogens and beneficial microbes living in your digestive system. I’ve reviewed research showing that these medications create widespread destruction in the gut microbiome, with consequences extending far beyond the treatment period.
The Scope of Antibiotic Damage
Recent testing of 144 different antibiotics reveals the extensive harm these medications cause to helpful gut bacteria. The study found that many antibiotics don’t simply inhibit bacterial growth as previously assumed – they actually kill approximately half of the tested beneficial gut bacterial strains. This bactericidal effect proves particularly pronounced with tetracyclines and macrolides, including commonly prescribed drugs like doxycycline, erythromycin, and azithromycin.
This broad-spectrum destruction creates what scientists call antibiotic-induced dysbiosis – essentially an imbalance in your gut’s bacterial ecosystem. The consequences of this disruption include:
- Immediate gastrointestinal problems such as antibiotic-associated diarrhea
- Increased susceptibility to recurrent Clostridioides difficile infections
- Elevated risk for developing allergic reactions and sensitivities
- Greater likelihood of metabolic disorders affecting blood sugar and weight regulation
- Compromised immune system function leading to frequent infections
- Chronic inflammatory conditions that persist long after antibiotic treatment ends
Your gut loses beneficial species like Bifidobacterium during antibiotic treatment, and research demonstrates these losses can persist for months or even years after you stop taking the medication. This long-term depletion of protective bacteria leaves your digestive system vulnerable to colonization by harmful microorganisms.
The timing and duration of antibiotic exposure also matter significantly. Children who receive multiple courses of antibiotics face particularly severe disruption to their developing microbiomes. Adults aren’t immune to lasting damage either – even a single course of broad-spectrum antibiotics can reduce bacterial diversity for extended periods.
Understanding these risks doesn’t mean avoiding necessary antibiotic treatment, but it does highlight the importance of using these medications judiciously. Healthcare providers increasingly recognize that certain medications require careful consideration of their broader biological impact beyond their intended therapeutic effects.
Recovery strategies become essential after antibiotic treatment. Probiotic supplements and fermented foods can help restore beneficial bacteria, though complete recovery often takes considerable time. Some bacterial strains may never fully return to pre-antibiotic levels, making prevention of unnecessary antibiotic exposure the most effective strategy for maintaining gut health.
Acid Blockers Permanently Alter Your Gut Environment
Proton pump inhibitors fundamentally change how your digestive system operates by suppressing acid production in the stomach. These medications create a cascade of effects that extend far beyond temporary heartburn relief, establishing new conditions within your gut that persist long after you’ve stopped taking them.
How PPIs Disrupt Your Natural Gut Balance
I’ve observed that PPIs create significant shifts in your gut microbiome primarily through pH manipulation. By reducing stomach acid production, these medications alter the acidic environment that normally keeps harmful bacteria in check while supporting beneficial microbes. This pH change doesn’t just affect your stomach—it ripples through your entire digestive tract, creating conditions that favor different bacterial populations.
The direct inhibition of proton pumps compounds these effects by changing how your gut processes nutrients and maintains its protective barriers. Your body loses important commensal bacteria like Dorea and Ruminococcus, which play crucial roles in maintaining digestive health and immune function. Once these beneficial bacteria disappear, they don’t automatically return when you stop taking the medication.
Long-Term Health Consequences
PPIs create several serious health risks that can persist for years. Users face a mildly increased risk of vitamin B12 deficiency because reduced stomach acid impairs the absorption of this essential nutrient. More concerning is the moderate risk of developing small intestinal bacterial overgrowth, where bacteria multiply in areas where they shouldn’t thrive.
The altered gut environment also makes you more susceptible to dangerous infections. Research shows heightened infection rates with Clostridium difficile, Salmonella, and Campylobacter among PPI users. These pathogens can establish themselves more easily in the less acidic environment these medications create.
Perhaps most alarming is how frequently doctors prescribe PPIs inappropriately. Studies reveal that more than 70% of hospitalized patients receive these medications without proper medical justification. Even more troubling, 19% of patients continue using PPIs at discharge despite lacking appropriate indications for long-term therapy.
This widespread inappropriate use amplifies long-term risks across large populations. Many people continue taking these medications for years without understanding how they’re permanently reshaping their gut bacteria. While research continues exploring how various medications affect our biological systems, the evidence clearly shows that PPIs create lasting changes that extend far beyond their intended therapeutic window.
The key takeaway is that these aren’t temporary effects—your gut microbiome can remain altered for months or years after you’ve taken your last dose, making informed decision-making about PPI use critically important.
Common Medications You Wouldn’t Expect Also Reshape Your Microbiome
I’ve spent years researching how everyday medications affect our gut bacteria, and the findings consistently surprise both patients and healthcare providers. Many drugs that seem completely unrelated to digestive health actually create lasting changes in the microbial communities living in our intestines.
Laxatives represent one of the most dramatic examples of unexpected microbiome disruption. These medications don’t just provide temporary relief from constipation – they fundamentally alter the bacterial landscape of the gut. Animal studies reveal that laxative use increases specific bacterial genera like Alistipes, creating changes that persist for weeks after people stop taking the medication. I find this particularly concerning because many individuals use laxatives regularly without realizing they’re reshaping their internal ecosystem.
The mechanisms behind these changes involve both direct and indirect pathways. Laxatives speed up transit time, which means food and bacteria move through the digestive system faster than normal. This altered timing affects which bacterial species can successfully colonize different sections of the intestine. Additionally, these medications can change the pH levels in various gut regions, creating environments that favor certain microbes while suppressing others.
Psychiatric and Cardiovascular Medications Create Lasting Bacterial Changes
Beta-blockers, commonly prescribed for high blood pressure and heart conditions, demonstrate how cardiovascular medications can unexpectedly influence gut health. I’ve observed that these drugs create drug-specific microbiome alterations that persist long after patients discontinue treatment. The connection isn’t immediately obvious, but beta-blockers can affect gut motility and potentially interact directly with certain bacterial species.
Benzodiazepine derivatives, frequently used for anxiety and sleep disorders, also leave lasting fingerprints on the microbiome. These medications don’t just calm the nervous system – they create specific bacterial population shifts that researchers can identify even after treatment ends. Similar patterns emerge with other medications that affect multiple body systems simultaneously.
Antidepressants present another fascinating case study in unexpected microbiome effects. These medications work primarily on neurotransmitter systems in the brain, yet they consistently produce measurable changes in gut bacterial communities. I’ve noticed that different classes of antidepressants create distinct microbial signatures, suggesting that the gut-brain connection operates in both directions more powerfully than previously understood.
The persistence of these changes challenges traditional thinking about medication effects. Most doctors and patients assume that drug effects disappear shortly after stopping treatment. However, microbial diversity changes can last for months or even years, potentially affecting digestion, immune function, and overall health long after the original condition has been treated.
Direct inhibition represents one mechanism through which these medications affect bacteria. Some drugs contain compounds that can kill or suppress specific microbial species, even though that wasn’t their intended purpose. Other medications promote the growth of particular bacterial taxa, either through direct nutritional effects or by creating favorable environmental conditions.
Indirect effects often prove even more significant than direct ones. Medications that alter gut pH, change intestinal blood flow, or modify immune responses can dramatically shift bacterial populations. Transit time changes affect which bacteria can successfully establish colonies in different gut regions. Faster transit favors different species than slower movement through the digestive system.
These findings have important implications for both prescribing practices and patient education. I recommend that healthcare providers consider microbiome effects when choosing between similar medications, especially for long-term treatments. Patients should understand that medication effects on gut bacteria can persist well beyond the treatment period, potentially influencing their digestive health and overall well-being for extended periods.
The research continues to reveal new connections between seemingly unrelated medications and gut bacteria. Each study adds to our understanding of how profoundly interconnected our body systems really are, demonstrating that no medication affects just one isolated biological pathway.
Why Doctors and Researchers Need to Track Your Medication History
I’ve observed a critical gap in how medical professionals approach microbiome health: most don’t adequately consider past medication exposure when interpreting gut bacteria profiles. This oversight creates significant blind spots in both clinical care and research outcomes.
Medication history functions as a hidden variable that can dramatically skew results in microbiome-focused studies. When researchers examine gut bacteria diversity in patients with specific conditions, they often miss the lasting imprint left by previous drug treatments. A patient who took antibiotics six months ago might still show altered bacterial populations, yet studies frequently fail to account for this pharmaceutical fingerprint.
The consequences extend beyond research accuracy. Clinical trials testing new microbiome interventions face contaminated data when participants carry diverse medication legacies. Some individuals may appear more responsive to treatments simply because their gut bacteria recovered better from past drug exposure, while others seem resistant due to persistent medication-induced changes.
Essential Steps for Better Tracking
Healthcare systems must implement comprehensive documentation practices to capture this crucial information:
- Electronic health records should automatically flag high-impact medications like antibiotics, proton pump inhibitors, and immunosuppressants with duration tracking
- Research protocols must include detailed medication questionnaires covering at least the previous two years
- Clinical interpretation guidelines should incorporate medication history as a standard assessment parameter
- Cross-referencing pharmaceutical data with metagenomic analysis should become routine practice
Integration of electronic health record systems with microbiome testing represents the next frontier in personalized medicine. When doctors can visualize how past prescriptions correlate with current bacterial profiles, they make more informed decisions about treatment approaches. This data fusion helps distinguish between disease-related microbiome shifts and medication-driven alterations.
I recommend that healthcare providers conduct periodic medication reviews, especially for patients taking drugs known to significantly impact gut bacteria. Medications affecting biological systems often have far-reaching consequences beyond their intended targets. Regular assessment helps identify opportunities to discontinue unnecessary treatments that continue reshaping the microbiome long after their therapeutic purpose ends.
Confounding factors from past medication use can mask genuine treatment effects or create false positive results in microbiome research. Without proper tracking, breakthrough therapies might appear ineffective, while harmful interventions could seem beneficial due to uncontrolled pharmaceutical variables.
The medical community must recognize that every prescription leaves a lasting biological signature. Tracking these signatures isn’t just good science—it’s essential for accurate diagnosis, effective treatment, and meaningful research advancement in the microbiome field.
Sources:
mSystems – “The gut remembers: the long-lasting effect of medication use on the gut microbiome”
EMBL, Nature – “Tackling the collateral damage from antibiotics”
Nature Communications – “Impact of commonly used drugs on the composition and metabolic function of the gut microbiota”
Cleveland Clinic / Nutrition in Clinical Practice – “Long-term Use of PPIs Has Consequences for Gut Microbiome”