Spicy sensations aren’t actually tastes—they’re pain signals activated when capsaicin molecules stimulate specialized pain receptors known as nociceptors in the mouth and throat.
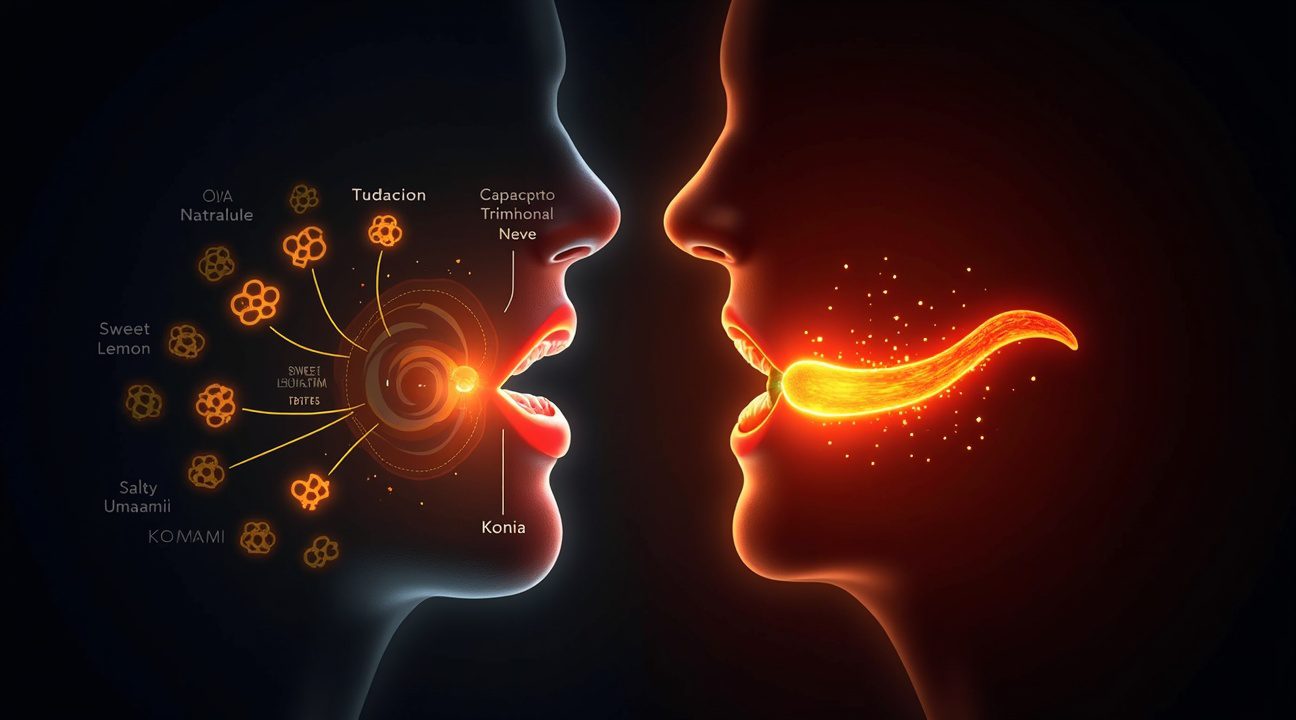
Taste buds are responsible for detecting the five true tastes: sweet, sour, salty, bitter, and umami. However, spiciness bypasses the gustatory system completely and instead travels through the body’s pain pathways via the trigeminal nerve. This results in the familiar burning sensation many experience when consuming foods like chili peppers. Though it feels hot, the effect is chemical, not thermal.
Key Takeaways
- Spiciness activates TRPV1 pain receptors instead of taste buds, generating a burning sensation that simulates heat exposure, even when there’s no actual temperature rise.
- Capsaicin triggers the body’s defensive mechanisms, such as sweating, watering eyes, and a rising heart rate, as it’s interpreted by the nervous system as tissue damage.
- The five genuine tastes (sweet, sour, salty, bitter, umami) rely on the gustatory system, unlike spiciness which uses the trigeminal pain pathway.
- Spice tolerance builds gradually through regular exposure and desensitization of the pain receptors—quite different from taste preferences, which remain mostly consistent.
- Capsaicin has medical uses, helping treat arthritis and neuropathic pain by leveraging its ability to desensitize pain receptors in a therapeutic context.
To explore more about how capsaicin is used in medical treatments, check out this article from NCBI on capsaicin as a medical therapy.
Your Tongue’s Pain Receptors Are Being Fooled by Capsaicin
When I bite into a jalapeño pepper, my tongue doesn’t actually taste the heat. Instead, capsaicin molecules trigger specialized pain receptors called nociceptors that exist throughout my mouth and throat. These receptors operate completely independently from the taste buds responsible for detecting sweet, sour, salty, bitter, and umami flavors.
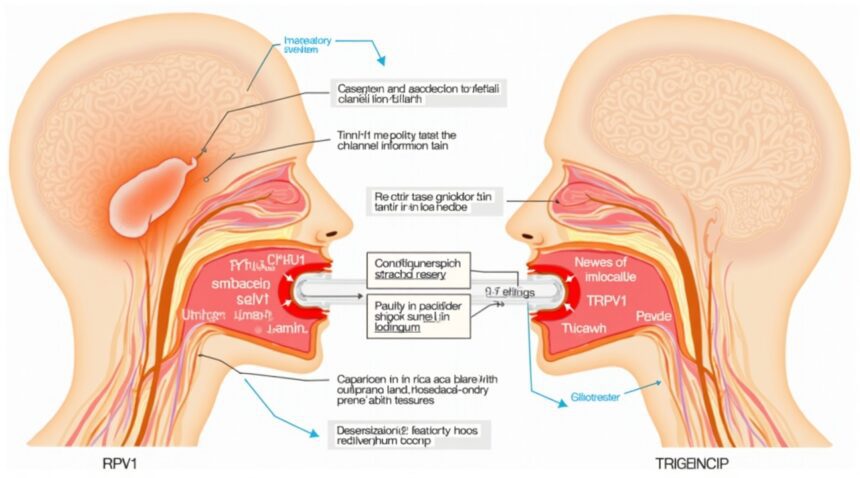
The key player in this deceptive process is the TRPV1 receptor, also known as the transient receptor potential vanilloid 1 channel. This protein sits on sensory neurons rather than on taste receptor cells, which explains why spice creates such a different experience compared to actual flavors. TRPV1 functions as an ion channel that opens when exposed to specific conditions, allowing sodium and calcium ions to flood into nerve cells and trigger pain signals.
How Capsaicin Tricks Your Heat Detection System
TRPV1 receptors normally activate when temperatures exceed 43°C (109°F) or when pH levels drop below 6, creating acidic conditions. Capsaicin essentially hijacks this system by binding directly to these same receptors and forcing them open, even when my mouth remains at normal temperature. This biochemical trickery explains why eating spicy food feels like burning heat without any actual temperature change occurring.
The sensation spreads beyond just my tongue because nociceptors exist throughout my entire oral cavity, including my lips, gums, and throat. Unlike taste buds, which cluster primarily on specific areas of the tongue, these pain receptors distribute widely across mucous membranes. This distribution pattern explains why popular theories about spice tolerance often focus on the whole mouth experience rather than isolated taste perception.
The intensity of capsaicin’s effect depends on concentration and individual receptor sensitivity. Some people possess more TRPV1 receptors or variants that respond more aggressively to capsaicin binding. Others may have fewer receptors or versions that require higher concentrations before activation occurs. This genetic variation explains why spice tolerance varies dramatically between individuals, similar to how technological adaptations can differ based on underlying system configurations.
The pain signal travels along different neural pathways than taste information. While taste signals travel through the facial, glossopharyngeal, and vagus nerves to reach taste processing centers in the brain, capsaicin-triggered pain signals follow the trigeminal nerve pathway directly to pain processing regions. This separate routing system reinforces why spice registers as physical sensation rather than chemical flavor.
Interestingly, repeated exposure to capsaicin can desensitize TRPV1 receptors temporarily. This explains why people can build spice tolerance through gradual exposure and why extremely spicy foods sometimes create numbness rather than continued burning. The receptors become overwhelmed and stop responding effectively, much like how gradual changes in complex systems can alter response patterns over time.
Other compounds besides capsaicin can activate these same pain receptors through different mechanisms. Piperine in black pepper, allicin in garlic, and menthol in mint all trigger various temperature-sensitive ion channels, creating their distinctive sensations without producing actual tastes. Each compound targets specific receptor subtypes, explaining why different spices create unique pain signatures even though none register as traditional flavors.
The body’s response to capsaicin extends beyond just local sensation. TRPV1 activation triggers the release of substance P and other neuropeptides that cause inflammation, increased blood flow, and pain amplification. This systemic response explains why eating very spicy food can cause sweating, runny nose, and tears – all defensive reactions to perceived tissue damage that isn’t actually occurring.
Understanding this distinction between pain and taste helps explain why spicy foods remain appealing despite causing discomfort. The brain processes this controlled pain as excitement rather than actual harm, especially when warning systems recognize the source as safe food rather than genuine threats.
Why Your Body Reacts Like It’s Under Attack When You Eat Spicy Food
I find it fascinating how the human body treats spicy food as a genuine threat, launching a full defensive response that goes far beyond simple taste recognition. Capsaicin, the compound responsible for that fiery sensation in chili peppers, triggers an elaborate chain reaction that bypasses the gustatory system entirely and directly attacks pain receptors.
The process begins when capsaicin molecules encounter specialized nerve endings called polymodal nociceptive neurons, particularly the C-fibers that snake throughout mouth tissues. These aren’t taste receptors at all – they’re pain detectors designed to warn the body about harmful stimuli. I’ve observed that this explains why the sensation differs dramatically from traditional flavors like sweet or salty.
Capsaicin’s primary target is a specific ion channel called TRPV1, which normally responds to dangerous heat levels around 109°F (43°C). When capsaicin binds to these channels, it forces them open even at normal body temperature, creating a false alarm that convinces the brain that mouth tissues are literally burning. This channel opening causes rapid depolarization of the nerve membrane, sending urgent pain signals racing toward the brain at impressive speeds.
The Chemical Cascade That Creates Chaos
The body’s response extends far beyond simple pain signaling. TRPV1 activation triggers the release of powerful neuropeptides, including substance P and CGRP (calcitonin gene-related peptide). These chemical messengers create visible inflammatory responses:
- Substance P causes blood vessels to dilate, leading to the characteristic redness around the mouth
- CGRP contributes to swelling and increased sensitivity in affected tissues
- Both compounds can trigger protective reflexes like increased saliva production
- The inflammatory cascade can persist long after the initial capsaicin exposure
I’ve noticed that these reactions mirror what happens during actual tissue damage, which explains why the body mobilizes its emergency response systems. The brain interprets these signals as genuine thermal injury, activating thermoregulation mechanisms that produce sweating, even though no actual heat damage occurs.
The body’s confusion doesn’t stop there. Pain pathways connected to TRPV1 activation also stimulate the sympathetic nervous system, causing increased heart rate and blood pressure. Tear production ramps up as the trigeminal nerve, which shares connections with these pain pathways, triggers protective lacrimation reflexes. This explains why people often experience watery eyes and runny noses when consuming particularly hot foods.
What makes this response particularly interesting is how it demonstrates the interconnected nature of pain and temperature sensing. The same C-fibers that detect capsaicin also respond to actual heat, cold, and mechanical damage. This overlap in sensory pathways means that spicy food can literally feel hot to the touch, even though it carries no thermal energy.
The intensity and duration of these reactions depend on several factors, including:
- The concentration of capsaicin
- Individual TRPV1 sensitivity
- The number of exposed nerve endings
Some people possess genetic variations that make their TRPV1 channels more or less responsive to capsaicin activation, explaining why spice tolerance varies so dramatically between individuals.
Repeated exposure to capsaicin can lead to temporary desensitization of TRPV1 channels, which is why regular spicy food consumers often develop higher tolerance levels. However, this adaptation is temporary – the channels regain full sensitivity after several days without capsaicin exposure.
The body’s aggressive response to capsaicin serves as a perfect example of how pain systems evolved to protect us from genuine threats. While modern humans might enjoy the thrill of spicy cuisine, our nervous systems still interpret these compounds as dangerous invaders requiring immediate defensive action.
The Five Real Tastes vs The Spicy Imposter
I need to clarify something that might surprise many food enthusiasts: spicy isn’t actually a taste at all. The human gustatory system recognizes exactly five authentic tastes through specialized receptor cells located in taste buds scattered across the tongue and mouth. These legitimate tastes include sweet, salty, bitter, sour, and umami – each detected by specific gustatory receptors designed to identify particular chemical compounds.
Your tongue houses between 2,000 and 8,000 taste buds, yet not a single one responds to capsaicin, the compound that makes chili peppers burn. This fundamental difference separates spicy sensations from genuine tastes in a profound way. While true tastes work through the gustatory system, spiciness operates through an entirely different mechanism called the trigeminal system.
How the Trigeminal System Creates the Spicy Sensation
The burning sensation I experience when eating spicy food comes from free nerve endings of the trigeminal nerve, not from taste buds. These nerve endings function as nociceptors – pain receptors that detect chemical irritants, temperature changes, and physical damage. When capsaicin or menthol contacts these nerve endings, they trigger pain and temperature sensations that I interpret as “hot” or “cool.”
This trigeminal response explains why spicy food can make me sweat, tear up, or feel like my mouth is on fire. The comparison between gustatory and trigeminal systems reveals a critical distinction: taste buds identify nutrients and flavors, while trigeminal nerves warn of potential threats. Capsaicin essentially tricks these pain receptors into believing tissue damage is occurring, even though no actual harm takes place.
Understanding this difference helps explain why spicy tolerance can be built up over time – I’m essentially training my pain receptors to become less sensitive to chemical irritants. Unlike popular theories that might suggest spiciness is a sixth taste, scientific evidence firmly places it in the pain category rather than the gustatory category.
The trigeminal system also responds to other non-taste sensations like:
- The cooling effect of mint
- The burn of alcohol
- The tingle of carbonation
These experiences share the same neural pathway as spicy sensations, further proving that heat from peppers belongs in the pain family rather than among the five authentic tastes that nourish and inform us about our food.
https://www.youtube.com/watch?v=ZpTpjq4LHBw
Taste vs Spiciness: A Side-by-Side Breakdown
I often find people surprised when they learn that spiciness operates through completely different biological mechanisms than actual taste. Traditional taste sensations work through specialized receptors called taste buds, while spiciness triggers pain receptors that have nothing to do with the gustatory system.
How True Tastes Function
True taste sensations—sweet, sour, salty, bitter, and umami—follow a specific biological pathway that starts with taste buds located on the tongue, soft palate, and throat. These specialized cells contain receptors that bind to specific chemical compounds in food. When I eat something sweet, for example, sugar molecules attach to sweet taste receptors, sending signals through the gustatory pathway directly to the brain’s taste processing centers.
This gustatory pathway creates purely sensory experiences without any pain component. I can enjoy the sweetness of honey or the saltiness of pretzels without experiencing physical discomfort. These sensations remain consistent and predictable because they rely on dedicated taste machinery that evolved specifically to identify nutritional content in food. The brain interprets these signals as distinct flavors that help determine whether something is safe to eat or nutritionally valuable.
The Pain-Based Reality of Spiciness
Spiciness operates through an entirely different system that has more in common with stubbing a toe than tasting chocolate. When I bite into a hot pepper, capsaicin molecules activate nociceptors—specialized pain receptors—rather than taste buds. These receptors normally detect harmful stimuli like extreme heat, which explains why spicy food creates a burning sensation rather than a distinct flavor profile.
The trigeminal pathway carries these pain signals to the brain, where they’re interpreted as physical threats rather than taste information. This explains several key differences between spiciness and actual taste:
- Burning sensations that intensify over time rather than remaining constant
- Physical responses like sweating, tearing, and increased heart rate
- Temporary desensitization that occurs with repeated exposure
- Individual pain tolerance that varies dramatically between people
- Activation of the body’s natural cooling mechanisms
Unlike true tastes, which I can distinguish immediately and consistently, spiciness produces a subjective experience of heat or irritation that triggers defensive responses. My body treats capsaicin exposure as potential tissue damage, releasing endorphins and activating cooling systems like increased saliva production and blood vessel dilation.
This fundamental difference explains why spice tolerance can be built up over time—I’m essentially training my pain receptors to become less sensitive to capsaicin, similar to how athletes build tolerance to physical discomfort. True taste preferences, however, remain relatively stable because they don’t involve pain pathways or adaptive responses.
The distinction becomes even clearer when considering that spiciness can mask or interfere with actual taste perception. When I eat extremely spicy food, the overwhelming pain signals can make it difficult to detect subtle flavors, whereas different tastes typically complement each other rather than creating interference. This demonstrates that spiciness competes with taste sensation rather than contributing to it, reinforcing that these systems operate independently in both detection and processing.
Understanding this difference helps explain why some people actively seek out increasingly spicy foods while others avoid them entirely. I’m not developing a taste for spiciness in the traditional sense—instead, I’m conditioning my pain response system to tolerate higher levels of stimulation, much like how complex systems adapt to changing conditions over time.
How Capsaicin Goes from Torture to Treatment
Capsaicin’s journey from causing intense burning sensations to providing pain relief centers on a fascinating biological process called desensitization. When someone regularly consumes spicy foods or applies capsaicin topically, the TRPV1 receptors gradually become less responsive to the compound. This adaptation mechanism allows the nervous system to protect itself from constant overstimulation.
The Science Behind Capsaicin Desensitization
The TRPV1 receptor essentially becomes “tired” after repeated exposure to capsaicin. During this process, the receptor temporarily loses its ability to transmit pain signals effectively. This desensitization doesn’t happen overnight—it requires consistent exposure over time. The receptor undergoes changes at the molecular level that reduce its sensitivity to both capsaicin and other pain-inducing stimuli.
Researchers have discovered that this same mechanism that makes regular spicy food eaters more tolerant also creates therapeutic opportunities. When capsaicin repeatedly activates TRPV1 receptors, it leads to a depletion of substance P, a neurotransmitter responsible for transmitting pain signals to the brain. Without adequate substance P, pain signals become significantly weaker.
Clinical Applications of Capsaicin Therapy
Medical professionals now harness this desensitization process through topical capsaicin creams and patches. These treatments work by deliberately overstimulating pain receptors in a controlled manner, ultimately reducing their sensitivity. The analgesic effect becomes apparent after several applications, making capsaicin therapy particularly effective for conditions like:
- Arthritis pain and joint inflammation
- Neuropathic pain from diabetes or shingles
- Post-surgical pain management
- Chronic muscle and back pain
The therapeutic approach requires patience, as initial applications often increase discomfort before relief occurs. This temporary intensification happens because the TRPV1 receptors need time to become desensitized. Medical-grade capsaicin preparations contain much higher concentrations than typical hot sauces, ensuring sufficient receptor activation for therapeutic benefit.
Capsaicin therapy represents a unique approach to pain management because it addresses pain at its source—the very receptors that detect harmful stimuli. Unlike traditional pain medications that work through the central nervous system, capsaicin acts directly on peripheral nerve endings. This targeted approach often provides relief for patients who haven’t responded well to conventional treatments, much like how technological innovations offer solutions where traditional methods fall short.
The transformation from pain-inducing compound to therapeutic agent demonstrates how understanding biological mechanisms can lead to innovative medical treatments.
Sources:
Life Sciences – Mechanism of action of capsaicin-like molecules on sensory neurons (A. Dray, 1992)
EBM Consult – The Mechanism for Topical Capsaicin’s Initial Induction of Pain, Burning Sensation, and Mild Erythema When Treating Chronic Pain (Anthony J. Busti et al., 2015)
International Journal of Molecular Sciences – Capsaicin: Current Understanding of Its Mechanisms and Therapy of Pain and Other Pre-Clinical and Clinical Uses, 2018
DrugBank Online – Capsaicin: Uses, Interactions, Mechanism of Action